Utilising digital health to improve medication-related quality of care for hypertensive patients: An integrative literature review
Kannikar Wechkunanukul, Daya Ram Parajuli, Mohammad Hamiduzzaman
Kannikar Wechkunanukul, College of Nursing and Health Sciences, Flinders University,Bedford Park 5042, Australia
Daya Ram Parajuli, Mohammad Hamiduzzaman, Flinders University Rural Health SA, College of Medicine and Public Health, Flinders University, Renmark 5341, Australia
Abstract
Key words: Hypertension; Digital health; eHealth; mHealth; Medication-related quality of care
INTRODUCTION
Hypertension or high blood pressure is considered as a significant contributor and risk factor to many serious conditions, including cardiovascular disease, brain, kidney and other medical conditions[1]. Approximately 1.13 billion people have hypertension globally, and it was a leading cause of 9.4 million deaths in 2010[1,2]. World Health Organization (WHO) reported a majority of hypertensive patients (80%) could not maintain their optimal blood pressure which can lead to complications such as heart attack, heart failure, stroke and kidney failure. A considerable effort has been made on improving the effectiveness of treatment and prevention to reduce the burden of disease and healthcare expenditure. One of the global targets is 25% reduction of the prevalence of hypertension by 2025 emphasised by the priority actions stated by WHO[2]. Some of the approach to achieving this goal includes establishing integrated programmes for treating hypertension, diabetes and other risk factors in primary care and promoting policies and programmes in education and encouraging adherence to medication treatment[2].
Hypertensive patients comorbid with other chronic conditions often present poor therapeutic outcomes due to complexity of the disease, medication non-adherence,poor medication management, drug interaction, and lack of self-management[3,4].Many pharmacist-led health care models in chronic conditions treatment have found associated with improving health outcomes[5,6]. There is an evidence from systematic reviews of effectiveness of medication management led by pharmacists[7]and efficient care system among multidisciplinary teams[8]play a crucial role in improving the medication-related quality of care (MRQOC) for example medication appropriateness and ultimately better cardiovascular health outcomes.
Technologies have become an inseparable part of the healthcare system for decades to help reducing the limitation of practices[9]. The innovations help to empower health professionals in many ways, such as optimal decision making and maintain a connection with patients and the healthcare team. Additionally, integrated technologies can upscale health provisions and improve the effectiveness of the healthcare system. WHO has recommended that the digital health interventions(DHIs) and the Health System Challenges should be used in tandem in addressing health needs such as using telehealth to increase accessibility in rural area or approach patients via short message services (SMS) to remind the follow up appointment[10]. To monitoring quality and effective of DHI, WHO has developed the classification of DHI version 1.0 in 2018[10]and the recommendations on digital interventions for health system strengthening covering interventions for healthcare providers, clients,health system managers, data services and research considerations[11,12]. The mHealth evidence reporting and assessment (mERA) checklist, and guidelines for reporting of health interventions using mobile phone has been developed by WHO mHealth Technical Evidence Review Group to establish the standard of reporting of mobile health[13]. These developments emphasise that we are globally transforming into the era of digital health care.
Recently, digital health or e-health interventions have been implemented widely into the healthcare system in many countries to improve MRQOC in various clinical and community settings, particularly for chronic disease management[14-16]. It is important to learn how those innovations implemented into practices and the outcomes from different approaches.
Therefore, this review aims to summarise the findings from a range of research investigating the use of digital health innovation to improve MRQOC for hypertensive patients.
MATERIALS AND METHODS
This is an integrative literature review which allows the inclusion of research evidence from a range of diverse methodologies including quantitative, qualitative and mixed methods approaches[17]. The summary of the existing empirical and theoretical literature was prepared to establish comprehensive evidence of the utilisation of digital health innovation, contributing to the improvement of MRQOC for hypertensive patients.
Information sources and search
A comprehensive search was undertaken in MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAH), and Scopus databases during October 2019 for relevant published articles written in English with no date restriction. The keywords used in the search included three main concepts. Concept 1 included “hypertension”,“hypertensive”, “HTN”, “HT”, “high blood pressure”, and “raised blood pressure”.Concept 2 involved “digital health”, “eHealth”, “mHealth”, “mobile health”,“innovation”, “intervention”, “initiative”, “model”, “program” and “digital health technology”. Concept 3 included “medication-related quality of care”, “MRQOC”,“medication”, “medicine”, “management”, “review”, and “transition care”.
To expand the search strategy, the Boolean operator “or” was used within each concept. Then the search terms in all concepts were combined with the Boolean operator “and” for a specific search. Reference lists of included articles were manually searched, and eligible articles were assessed against the inclusion criteria. Search results were then imported into an EndNote X9 Library. The pooled search results in the EndNote X9 Library were checked for duplicated records and removed where appropriated.
Eligibility criteria
The inclusion criteria for this review were: (1) Types of participants: Studies that included primary analysis or secondary analysis of patients with hypertension. This review included all relevant studies with no specific age, gender, comorbidity or ethnicity of participants; (2) Types of intervention/interest: Studies that investigated the effectiveness, efficacy, feasibility of DHI/program/model for hypertension care or management. Also, studies that examined the association between DHI/program/model and the MRQOC for hypertensive patients were included; (3) Types of studies: Original research deployed quantitative or mixed methods approaches within level I to level IV of the National Health and Medical Research Council(NHMRC) evidence hierarchy[18], including experimental or quasi-experimental studies, and observational studies. The study included studies irrespective of any settings. This review excluded any types of review or meta-analysis articles; and (4)Types of outcomes: Studies that measured any indicators of MRQOC[19]for hypertensive patients, including medication appropriateness in hypertension, general medication appropriateness, detection and monitoring of adverse events, and access to collaborative health services (e.g., medication review, and annual cycle of care for people with chronic disease).
Methods of review
This review was conduct ed comprehensively in accordance with guidelines and checklist for writing an integrative review[17,20]Additionally, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines and checklist for the reporting of systematic reviews was used to ensure the quality of the report[21].Eligible articles were assessed independently by two reviewers (KW and DRP). Any conflicts that arose between the reviewers (KW and DRP) were resolved through discussion, or with a third opinion (MH).
Data extraction and synthesis
The data reduction was performed through classifying selected studies based on research designs defined as the level I to level III of the National Health and Medical Research Council (NHMRC) evidence hierarchy, including randomised controlled trials (RCT), pseudo-randomised controlled trials, and comparative studies, including randomised controlled trials and comparative studies[18]. Relevant data were extracted from all included articles and managed on a spreadsheet using Microsoft Excel?spreadsheet software (KW, DRP and MH). The extracted data were analysed and presented in tabular form comparing variables of interest, including digital intervention elements, reduction in systolic blood pressure, and MRQOC, challenges of implementing digital intervention for hypertension care (KW, DRP and MH).Finally, the outcomes of data syntheses were presented in Tables 1, 2, 3, and 4 (KW,DRP and MH).
RESULTS
Selection and characteristic of selected studies
The comprehensive search in the databases yielded a total of 115 relevant articles. The three duplicated records were removed, and 69 records were excluded by title/abstract. The 43 full-text articles and three additional articles derived from the hand search were subsequently included for eligibility assessment (n =46). A total of 18 records did not meet the inclusion criteria and were excluded, leaving 28 articles were included in the review (Figure 1).
A total of 18433 participants from 28 articles were included in this review (Table 1).Sample size varied across the reviewed studies between 18[22]and 6061[23]participants.The average mean age of participants involved in 15 interventions was 59, ranging from 42[22]to 81[24]years old. The proportion of male participants ranged from 13.9%[25,26]to 92.0%[27]with eight interventions had males as a predominant gender as over 50% of participants of individual study. The average mean systolic blood pressure (SBP) at baseline of all reviewed studies was 143.3 mmHg, ranging from 129.0 mmHg[27]to 159.0 mmHg[28].
Methodological quality
There were 19 digital interventions identified from these 28 articles. Eight research designs were identified: Nine randomised controlled trials (RCT); two cluster RCTs;four pre-post studies; one mixed methods design; one cohort study; one quasiexperimental study; one retrospective study; and one cross-sectional study. These DHIs were conducted in eight countries, including United States (nine interventions,16 publications); Canada (three interventions); India (two interventions); Lebanon(one intervention, three publications); and one intervention in the following countries:United Kingdom, South Korea, Pakistan, and Australia. The follow up were performed for RCT and pre-post studies ranging from 2[29,30]mo to 18[23,31]mo with the average attrition rate of 10.1%, ranging from 0.0%[22,29]to 17.4%[25,26]. The summary of the included publications is presented in Table 1.
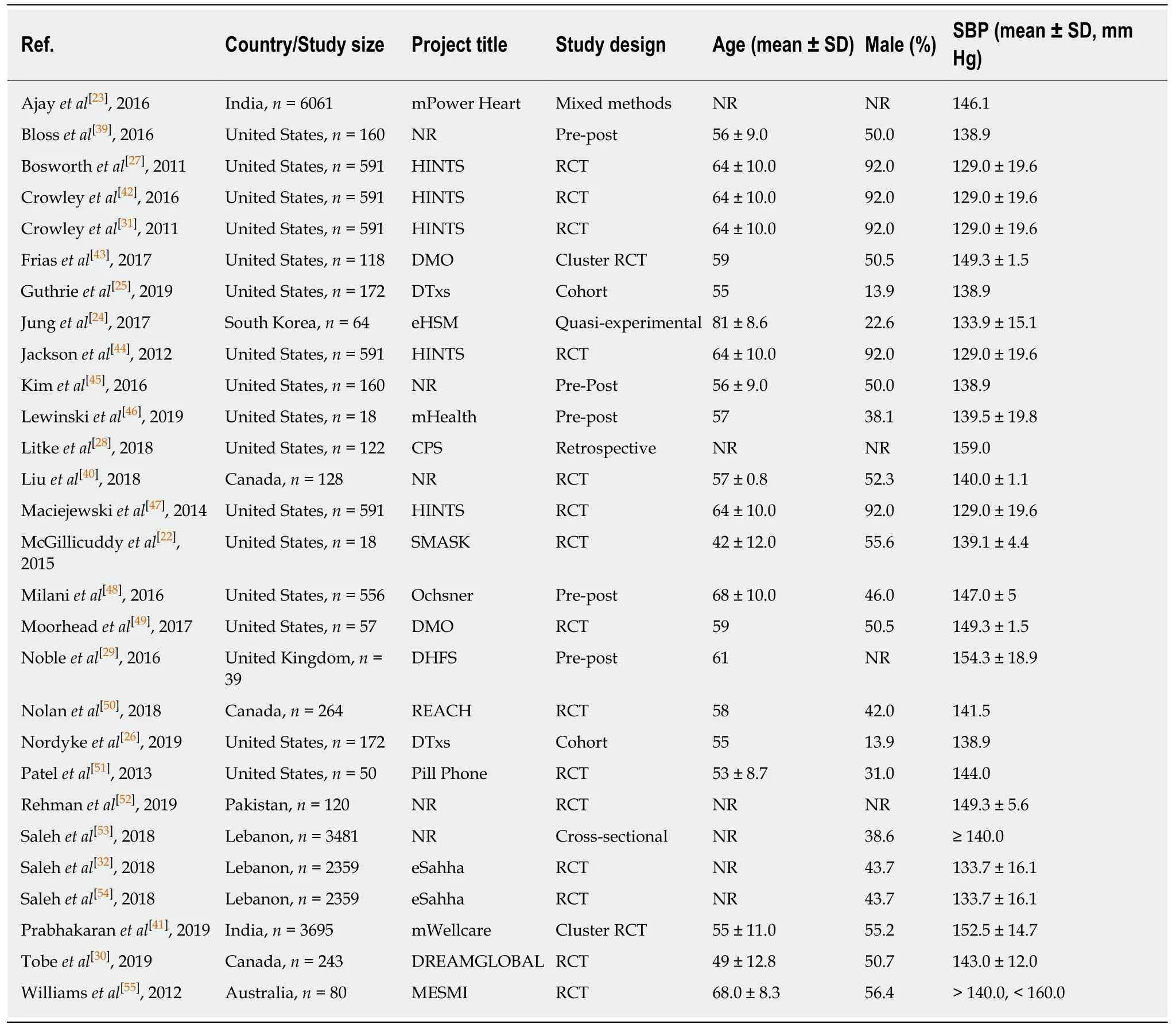
Table 1 Summary of included articles
All reviewed studies performed statistical tests appropriately. The mean with standard deviation or median with Interval Quartile Range were used to present continuous variables andt-test or Mann-WhitneyUtest were used for comparisons.Percentage, frequency, and Chi-square test were used as statistical tests relevantly for categorical variables. The statistical models were used appropriately to test the effect of interventions or association between variables. The thematic analysis were used for qualitative data and presented as a narrative format accordingly.
DHIs
There were 19 DHIs included in this review. The main elements of each intervention are presented in Table 2. Eight interventions were conducted in rural areas, five intervention were delivered specifically in urban areas, whereas the remaining six interventions were provided to general population. Study sites varied from clinicalbased settings, community-based settings to home-based program, and the majority of DHIs were conducted at primary care settings. These interventions were used by health professionals, patients or both parties through different technologies, including mobile phone (n =5), mobile health system (n =4), short message service (n =3), and telehealth (n =3), digital medicine (n =2), and the internet (web-based) (n =2).Reducing blood pressure among hypertensive patients was the most common objective of all reviewed interventions, followed by improving self-management,medication adherence, medication management, health behaviour modification (i.e.,lifestyle, physical activity and diet) and accessing healthcare. There were multidisciplinary team from different sectors involving in DHI developments and implementations: Researchers, research bodies, healthcare providers, health professionals, public and policy makers, health insurance providers, technology developer and patients. Majority of interventions recruited hypertensive patient comorbid with other chronic diseases such as type 2 diabetes and dyslipidaemia.
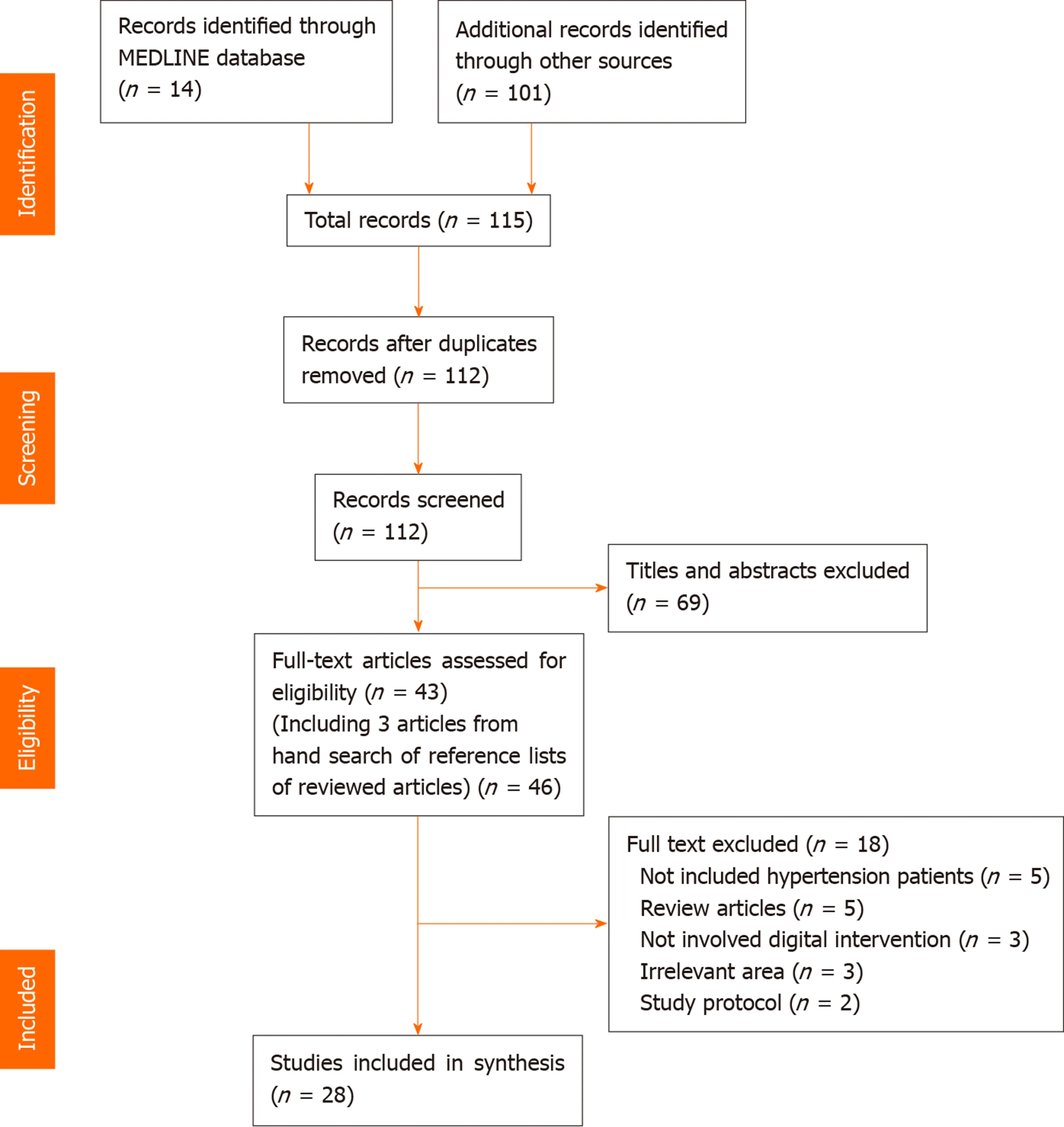
Figure 1 Selection flow diagram.
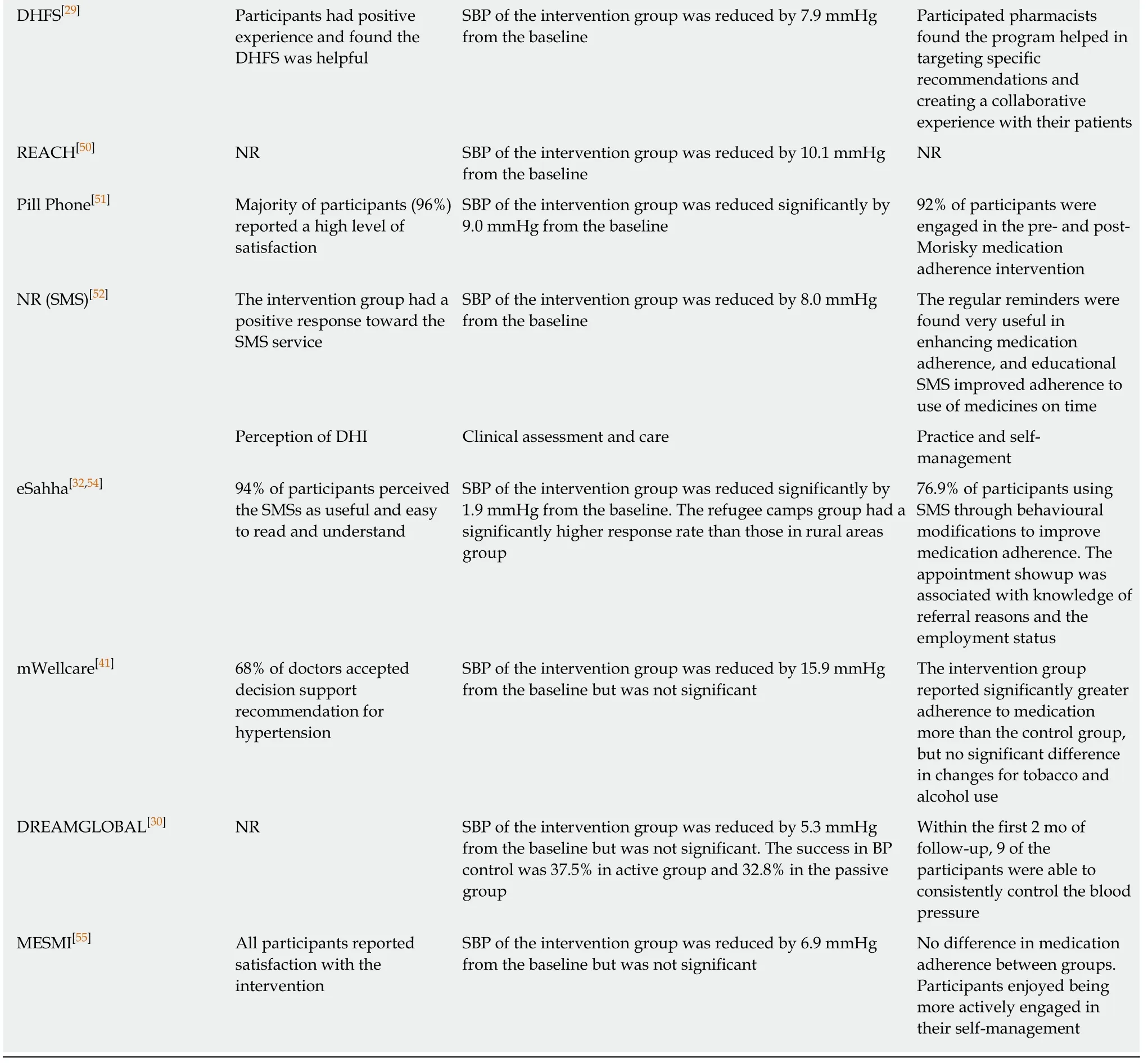
MRQOC
Twenty-seven articles measured blood pressure or blood pressure control as the primary outcomes of DHI and compared to the usual care. The reduction of SBP ranged between 1.9 mmHg[32]and 26.0 mmHg[28], with a mean of 10.81 mmHg. Other outcomes were measured to examine the effectiveness or feasibility of DHIs for hypertensive care in different settings. Utilising digital health were found positively impacted on the MRQOC for hypertensive patients, including improving medication adherence and medicatio n management; reducing adverse drug events; increasing medical review; improving blood pressure control; detecting complication; increasing opportunistic screening of hypertension; maintaining follow up appointment and management plan review; encouraging self-management and health behaviour modification (i.e., lifestyle, physical activity and diet); increasing access to healthcare particularly among patients living in rural area. However, some interventions found no significant impact of DHI for hypertensive care compared to the usual care. There were some inconsistent outcomes across these reviewed interventions either the same digital tool or between variations. Summary of findings derived from the 19 reviewed DHI is presented in Table 3 and challenges of implementing DHI for hypertension management is presented in Table 4.
DISCUSSION
This review summarised the findings from 28 research articles investigating in the useof digital health innovation to increase the MRQOC in hypertension management.There were 19 DHI developed differently with distinguishing elements based on aims and objectives of each projects. Eighteen interventions showed evidence of blood pressure reduction and improvement of self-management in relation to medication adherence and blood pressure control. These outcomes revealed the advantages of implementing DHI into healthcare practice for hypertension and some common chronic diseases which is consistent with previous reviews[33,34]. Despite the common benefits, inconclusive findings were found in some interventions and inconsistent outcomes between DHI were noted.
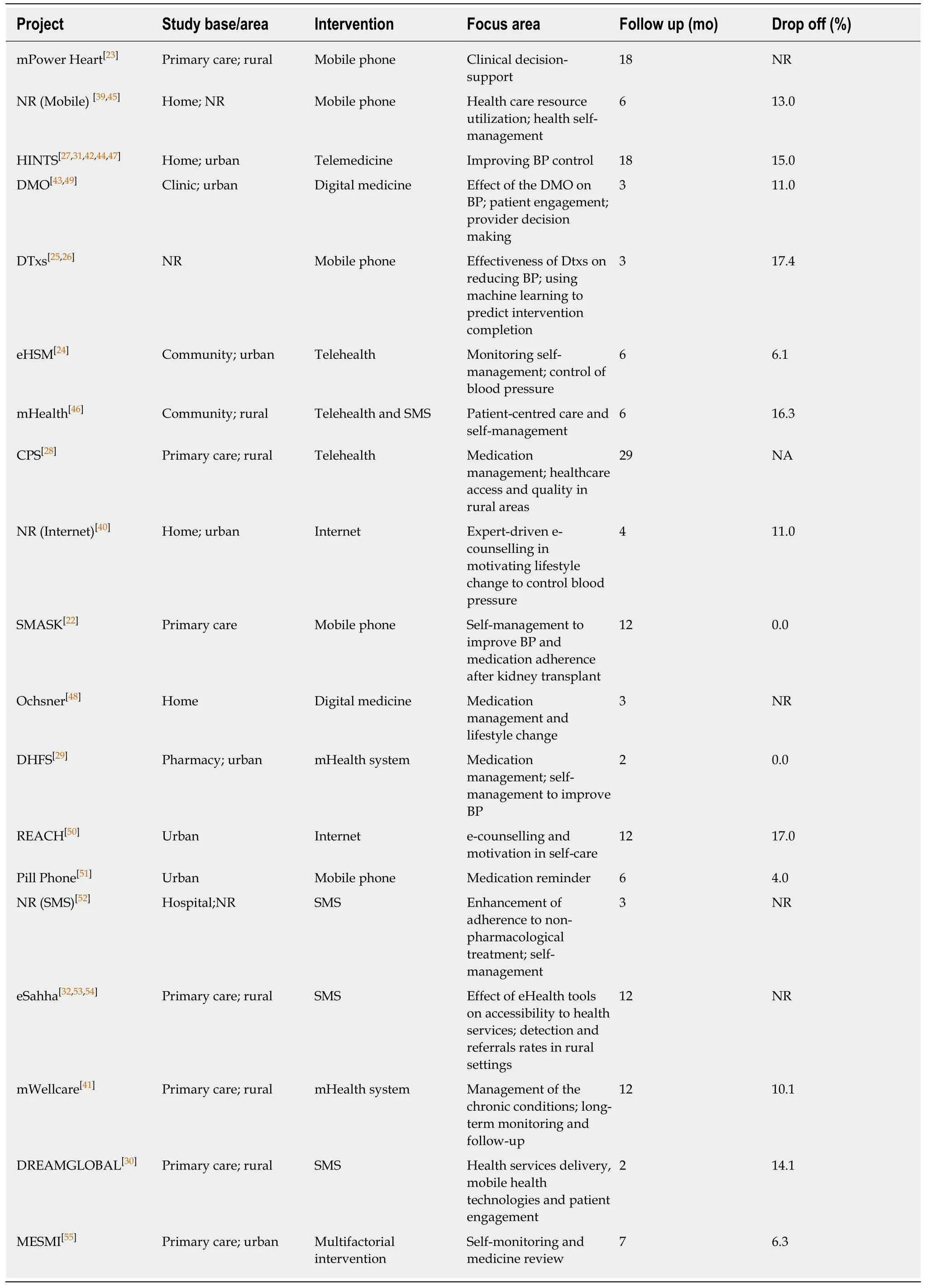
Table 2 Comparison of main elements between digital health interventions for hypertensive care
DHI: Digital health intervention; NR: Not report; BP: Blood pressure; SBP: Systolic blood pressure; HINTS: Hypertension Intervention Nurse Telemedicine Study; CPS: Clinical pharmacy specialists; DMO: Digital medicine offering; eHSM: eHealth self-management; SMASK: Smartphone Medication Adherence Saves Kidneys; DHFS: Digital health feedback system; SMS: Short Message Service; DTxs: Digital therapeutics; MESMI: Medication Self-Management Interventio.
The main focus of the included interventions ranged from clinical outcome; selfmanagement; quality use of medicine; to accessibility of care, play a key role in development and design of the DHI such as mobile application, telemedicine, digital medicine, SMS, mobile health system, and web-based program. Another salient factor is funding and sponsorship of the DHI project. The competitive market in pharmaceutical industry make the opened opportunity for certain DHI project, but it might come with conflicts of interest and bias inevitably. The objectives of each project may shape the design, scope, content, delivery method, and users of the DHIs as well. For example, the medication administration or appointment reminder would involve timing and organiser tools that can create individual preference and link with health professional through healthcare system, or their clinic calendar. Types ofinterventions (e.g., educational, informational, monitoring) and settings (e.g.,rural/urban, community, home, primary health care or clinical settings) seem to be an important consideration on digital device and platforms (e.g., mobile application,telephone, internet, SMS, or health system); and mode of delivery (e.g., in-person,remote mode, active/passive activity, and one-way/two-way direction). In brief,specific goal of health program, diversities of settings, population, available resources(e.g., human resource, funding) and sociocultural factors should be integrated into the early stage of project plan and design.

Table 4 Challenges in implementing digital health intervention for hypertensive patients
Although effectiveness of the DHI in various settings and population have been reported, growing body of literatures have identified key challenges for implementation and sustainability. Availability of resources[35], sustainability and user acceptance[36], technological issues and machine learning[37], digital illiteracy, inequities in access to healthcare, defined protocol to share information, and collaboration of stakeholders[38]were the major barriers in previous studies.
These challenges are in consistent with the summary of this review described in Table 4. To emphasize, implementing DHI for hypertension management or other chronic diseases may encounter some challenges depending on various factors of each program. A lack of resources, including digital tools (e.g., mobile phone, computer,network, software and technological devices), physical setting, and funding, could impede the progress of DHI, particularly in rural and remote areas[23,32,39]. Experts and partnerships play a crucial role in driving health interventions to reach the goals.Shortage of staff equipped with the skill set necessary to develop and implement DHI,and a weak collaboration between stakeholders could lead to unsuccessful outcome[39-41]. Despite the connection among professionals, patient engagement and relationship between providers and users is a cornerstone of all programs.
WHO Guide: Recommendation on DHI for research consideration[12]and healthcare system[11]have just launched in 2019. Many DHIs conducted prior exist of this recommendation was developed based on aims and objectives of the project and relied on the knowledge and experiences of research team which might involve various stakeholders such as researchers, health professionals, public health agencies and policy makers, technology industry (developers and suppliers), pharmaceutical company, health insurance providers and funding bodies. The WHO (2019)recommends several sets of implementation considerations for DHIs based on its specific contexts and conditions reflecting the evidence on effectiveness, acceptability,feasibility, resource use, equity and human rights. Utilising these specific recommendations would help enhance the achievement of translating DHI into practice.
The future DHI should be developed in concordance with these WHO recommendations to ensure the standard of DHI in healthcare and leading to a high quality and reliable outcomes. In addition, using guidelines to report the DHI such as guidelines for reporting of health interventions using mobile phones: Mobile health(mHealth) evidence reporting and assessment (mERA) checklist[13]will facilitate the standard of research in this area.
Although there exist some challenges of implementing DHI, the average attrition rate of selected studies was reasonably low at 10.1% which demonstrate a “willing”sense of engagement from diverse communities. Additionally, the positive perception of using digital tools among patients and health professionals emphasise the“welcome” of digital innovation into the healthcare system. These success experiences can be used as inspiration encouraging researchers, health professionals, funding bodies and other stakeholders to collaborate on digital health areas.
Limitations
This review adopted integrative review methods which may not be able to provide strong evidence in the effectiveness of the DHI due to heterogeneity of methodology of the original studies. However, this review involved 28 literature from eight countries across the globe, revealing some important outcomes of different types of DHI from different contexts. The outcomes of this review summarised from only 19 interventions may not reflect all contexts globally. However, there are pieces of knowledge established for a future study and practice.
The digital health innovation for hypertensive care in various contexts affected positively on MRQOC, leading to the improvement of patient outcomes and their quality of life. Nevertheless, inconclusive findings were found in some interventions,and inconsistent outcomes between DHI were noted. The findings of this review can be fundamental data for digital initiatives. A future DHI for hypertension or chronic diseases should be developed in accordance with WHO recommendations and the evidence-to-decision framework to warrant the sustainability and long-term effectiveness of on healthcare practices and patient outcomes. Additionally, a systematic review and meta-analysis looking at the effectiveness and costeffectiveness of digital health innovation in hypertension and chronic disease is warranted to establish a more comprehensive and concrete evidence-based practice.
ARTICLE HIGHLIGHTS
Research background
The global burden of hypertension has an upward trend and taken a huge part of healthcare expenditure. Recently, over a billion people are living with hypertensive condition, but only 20%of them can maintain their optimal blood pressure. The research evidence revealed positive outcomes of medication management models on improving the medication-related quality of care (MRQOC) such as medication appropriateness and health care accessibility. Digital health interventions (DHIs) have been utilised to improve quality of care for hypertension and to reduce the inequalities and accessibility in healthcare system.
Research motivation
Recently, DHIs have been implemented widely into the healthcare system in various settings to improve the chronic disease management, including hypertension. Nonetheless, the reports of those DHI varied from study to study based on the heterogeneity of methodologies, the different approaches and variety of technologies. Therefore, it is necessary to consider “lesson and learn”from existing DHIs implemented in hypertension care to improve patient outcomes and design future studies.
Research objectives
This review aims to summarise the outcomes from a range of research which investigated the use of DHI to improve the MRQOC for hypertensive patients.
Research methods
A comprehensive search was undertaken in MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Scopus databases during October 2019 for relevant published articles written in English with no date restriction. Quantitative or mixed methods studies within level I to level IV of the National Health and Medical Research Council evidence hierarchy, that measured any outcome for medication management for hypertensive patients, conducted in different settings were included in our review.
Research results
In total, 19 DHIs implemented in different countries were included. The variety of DHI were provided as community-based, clinical-based and home-based program through mobile phone,mobile health system, short message service, and telehealth, digital medicine, and online healthcare (web-based). This review revealed that utilising DHI for hypertensive care in different settings positively impacted on MRQOC leading to an improvement of patient outcomes such as blood pressure control, improvement in medication adherence and medication management,maintaining follow-ups, access to healthcare particularly in rural area and their quality of life.Nevertheless, inconclusive findings were found in some interventions, and inconsistent outcomes between DHI were noted.
Research conclusions
DHI for hypertensive care in different settings positively impacted on MRQOC. However, the inconsistent outcomes between studies are likely due to the heterogeneity of DHI. The findings of this review can be fundamental data for digital initiatives and lead to the evidence -based practice. A future DHI for hypertension or chronic diseases should be developed in accordance with WHO recommendations and the evidence-to-decision framework to warrant the sustainability and long-term effectiveness of on healthcare practices and patient outcomes.
Research perspectives
A future research in this area is warranted and DHI for hypertension should be developed through the evidence-to-decision framework and guidelines. A systematic review and metaanalysis looking at the effectiveness and cost-effectiveness of digital health innovation in hypertension and chronic disease is warranted to establish a more comprehensive and concrete evidence-based practice.
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Tumor circulome in the liquid biopsies for digestive tract cancer diagnosis and prognosis
- Isoflavones and inflammatory bowel disease
- Cytapheresis for pyoderma gangrenosum associated with inflammatory bowel disease: A review of current status
- Altered physiology of mesenchymal stem cells in the pathogenesis of adolescent idiopathic scoliosis
- Association between liver targeted antiviral therapy in colorectal cancer and survival benefits: An appraisal
- Peroral endoscopic myotomy for management of gastrointestinal motility disorder
