Like father, like son: Pulmonary thromboembolism due to inflammatory or hereditary condition? Two case reports
Pedro Hannun, Walter Hannun, Hugo Hyung Yoo, Lucilene Resende
Pedro Hannun, Hugo Hyung Yoo, Lucilene Resende, Department of Internal Medicine, Botucatu Medical School, S?o Paulo State University - UNESP, S?o Paulo 18618-687, Brazil
Walter Hannun, Department of Institutional Relations, Santa Catarina Hospital, S?o Paulo 01310-000, Brazil
Abstract BACKGROUND Venous thromboembolism, which includes deep venous thrombosis and pulmonary embolism, is a well-known causal disorder with high morbidity and mortality rates. Inherited or acquired conditions affecting components of coagulation and fibrinolysis systems have been linked to venous thromboembolism pathogenesis as they may lead to a pro-inflammatory state in human bodies. Toxoplasmosis is a zoonosis that potentially leads to acute systemic cachectic-inflammatory effects in experimental animal models but is not yet proven in humans. It is known that venous thrombosis can occur during acute inflammatory/infectious diseases, although it is not well established with regard to toxoplasmosis alone.CASE SUMMARY A 70-year-old Caucasian man and his 32-year-old son developed general malaise,chills, fever, and myalgia, having established a diagnosis of toxoplasmosis.Twenty days later, they presented dry cough leading to further investigations that revealed an incidental deep venous thrombosis plus pulmonary embolism in them both. Thrombophilia screening showed both patients had a factor V Leiden mutation heterozygosis. Father and son completely recovered without any sequalae after anticoagulant treatment. They have not presented symptom recurrence of either medical disorder during 1 year of follow-up.CONCLUSION Toxoplasmosis may enhance the risk of venous thromboembolism in patients showing factor V Leiden mutation heterozygosis.
Key Words: Factor V Leiden mutation; Thrombophilia; Venous thromboembolism; Deep venous thrombosis; Toxoplasmosis; Inflammation; Case report
INTRODUCTION
Inflammation and coagulation are intrinsically related processes that communicate at various levels; either can be the cause or consequence of the other[1,2]. The mechanism that links inflammation (originally infectious or not) and thrombosis is complex and not fully understood. The most commonly accepted hypothesis states that aseptic inflammations or infection-related inflammations promote the secretion of several cellular mediators, mostly related to the innate immune response. Inflammation activates endothelial cells, leukocytes, and platelets, resulting in cell dysfunction and/or injury and platelet aggregation[2]. Concomitantly, an infection can result in antiphospholipid antibodies that trigger the overproduction of tissue factor and thromboxane A2[3]. All together this could initiate the blood clotting cascade[1,2].
Toxoplasmosis, a common zoonosis caused by theToxoplasma gondiiprotozoan, is a systemic infection that may cause cachectic-inflammatory effects in experimental animal models[4] and even the development of antiphospholipid syndrome in humans[3,5]. Hence, toxoplasmosis by itself might eventually provoke a venous thromboembolism (VTE) event in a given patient.
In addition to having toxoplasmosis, our studied patients carried factor V Leiden(FVL) mutation heterozygosis, a well-known cause of thrombophilia. The combination of these two morbid conditions might have increased the risk of VTE in both patients.
CASE PRESENTATION
Chief complaints
A 70-year-old Caucasian man and his 32-year-old son had developed general malaise,chills, fever, and myalgia. Dry cough appeared approximately 20 d after initial symptoms in both patients.
History of present illness
At the beginning of 2019, a 70-year-old Caucasian man and his 32-year-old son had lunch together at a steakhouse in S?o Paulo City, Brazil. After 5 d, the older man developed general malaise, chills, fever, and myalgia; he also noticed enlarged cervical and occipital lymph nodes. One week later, he took a 10 h flight to the United States remaining abroad for 10 d without any clinical improvement. During this time, his son who had stayed in Brazil, started having similar symptoms. About 20 d later they both developed a persistent dry cough. One month after initial symptoms, they were hospitalized after being radiologically diagnosed with pulmonary thromboembolism.
History of past illness
The older man had a prostatic carcinomain situoperated 5 years earlier; he was also a former smoker.
The younger had only a right shoulder capsuloplasty 9 years earlier; he was a nonsmoker.
Personal and family history
The older man had current controlled hypertension and type II diabetes. There was no history of family disorders.
Physical examination
The relevant findings were enlarged cervical and occipital lymph nodes in both patients and muscular stiffness in the right calf of the younger man.
There were no respiratory signs or low oxygen saturation levels on room air.
Laboratory examinations
The following laboratory tests were normal in both patients: Blood cell count,prothrombin time, activated partial thromboplastin time, four hereditary alterations for thrombophilia (protein C, protein S, and antithrombin serum levels; G20210A prothrombin gene mutation search), and three acquired alterations for thrombophilia(anticardiolipin antibodies, anti-beta- 2-glycoprotein I antibodies, and lupus anticoagulant).
Tests with abnormal results in both patients were (Table 1): Presence of high serum C-reactive protein, presence of positive IgM antibodies forToxoplasma gondii, and presence of FVL mutation heterozygous status (gene F5, c.691G>A, p.R506Q).
D-dimers were only analyzed in the older patient with a high result.
Imaging examinations
Imaging studies are shown in Table 1.
In the father, pulmonary computed tomography angiography showed bilateral pulmonary embolism (Figure 1A), and a further Doppler ultrasound (US) found deep venous thrombosis (DVT) in the left lower limb (anterior tibial, posterior tibial, and fibular veins). In the son, pulmonary computed tomography angiography and Doppler US respectively showed a bilateral pulmonary embolism (Figure 1B) and DVT in the right lower limb (anterior tibial, posterior tibial, fibular, and popliteal veins).
FINAL DIAGNOSIS
The final diagnosis of both patients was identical, corresponding to pulmonary VTE associated with acute toxoplasmosis plus FVL heterozygous mutation status.
TREATMENT
Although clinically stable, both patients were admitted to the hospital to start anticoagulant therapy with enoxaparin (60 mg, subcutaneously, twice a day for 4 d)followed by rivaroxaban (15 mg, orally, twice a day) according to local standards.They were discharged completely free of symptoms, under oral anticoagulation for 1 year.
Regarding toxoplasmosis, treatment of immunocompetent adults with lymphadenopathic toxoplasmosis is rarely indicated due to its usually self-limited evolution[6].The only prescription being bed rest.
OUTCOME AND FOLLOW-UP
Father and son have totally recovered without sequelae. After 1 year of follow-up,patients have not presented a recurrence of either morbid condition.
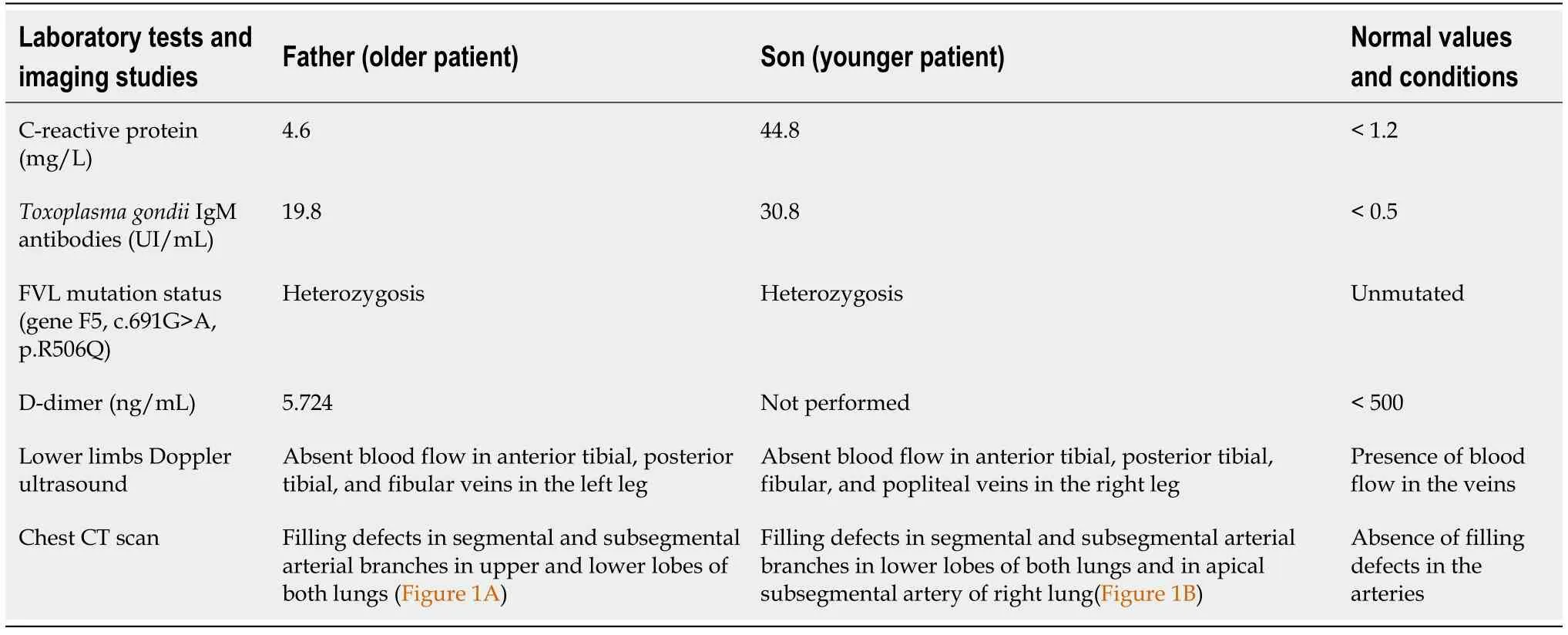
Table 1 Laboratory tests and imaging studies for both patients showing altered findings
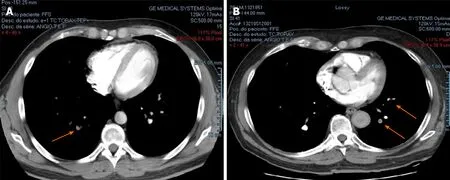
Figure 1 Pulmonary computed tomography angiography. A: Father’s pulmonary computed tomography angiography transversal slice of lungs showed filling defects in subsegmental arterial branches characterizing left pulmonary embolism (arrows); B: Son’s pulmonary computed tomography angiography transversal slice of lungs showed right pulmonary embolism (arrow).
DISCUSSION
Toxoplasmosis is a usually asymptomatic zoonosis with wide geographical distribution. According to the S?o Paulo Sanitary Surveillance Agency, at the beginning of 2019 there was an increased number of acute toxoplasmosis cases in S?o Paulo City,including asymptomatic cases only detected by positive serological tests due to a foodborne disease outbreak. Of the 165 notified cases, only 9% had severe complications, none being DVT or pulmonary embolism[7].
The relationship between toxoplasmosis and venous thrombosis is uncertain. There is evidence of direct[8,9] and indirect[3,5] toxoplasmosis effects that may lead to thrombotic events. Toxoplasmosis was described as resulting in cerebral vein thrombosis in severe cases of its congenital form in humans[8]. Placental thrombosis was also seen in abortions during experimentalToxoplasma gondiiinfection in sheep[9]. However, indirect toxoplasmosis effects have been more consistently reported in literature, especially human Toxoplasma-induced antiphospholipid syndrome[3,5].However, our studied cases did not show positivity for any antibodies related to antiphospholipid syndrome.
Being a systemic infectious disease, the potential for toxoplasmosis to trigger a venous thrombosisviaan inflammatory pathway cannot be neglected[1,2], especially in patients with FVL mutation heterozygous status, the most common type of inherent thrombophilia[10]. In association with a pre-existing prothrombotic state, the inflammatory and pro-hemostatic environment caused by the infection may have caused endothelial dysfunction and changes in coagulation homeostasis resulting in VTE[2].Considering a scenario without direct endothelial damage, it is also possible that the inflammation itself had increased the genetic expression of tissue factor (factor III),thus initiating the extrinsic coagulation pathway[2]. These two hypothetical situations would favor activation of mutated factor V, therefore amplifying thrombus formation given the mutated factor V resistance to activated protein C[2].
Some experimental and clinical studies corroborate the interaction between congenital thrombophilia and systemic infections/sepsis leading to exacerbation of thrombotic activity[11-13]. Although they differ regarding the impact of the thrombophilia gene mutation heterozygosis on survival of infected individuals, most agree that there is a significant increase in thrombin generation markers and in the conversion of fibrinogen to fibrin, both of which represent more frequent and severe episodes of thrombosis[11-13].
Regarding other predisposing factors for DVT, only the older of the two patients had a long period of immobility during a flight concurrently with toxoplasmosis. It is also important to highlight that both patients had undergone previous surgeries with no venous thrombosis.
Considering father and son had been living with the FVL heterozygous mutation throughout their lives without any thrombotic events, it does not seem a simple coincidence that they both simultaneously had VTE with concurrent toxoplasmosis.
CONCLUSION
This paper reports the unusual clinical cases of two closely related patients carrying the hereditary thrombophilia FVL heterozygous mutation who have concomitantly experienced the so far only VTE episode during concurrentToxoplasma gondiiacute infection. Their sharing of these three events does not seem to be mere coincidence and suggests a potential synergistic effect between toxoplasmosis and heterozygous mutation state for FVL as triggers of the thromboembolic events.

