The establishment of pancreatic islet isolation in India – an update on human pancreatic islet transplantation
Nithyakalyani Mohan, Srividhya Raghavan, Anusha Sunder, Anil Vaidya, Nivash Chandrasekaran, Senthil Muthuraman, Dinesh Babu, Karthik Mathivanan,Elan Krishnan,Balamurugan Appakalai
1Transplant and Research,Apollo Hospitals,Chennai,India.2Molecular Biology Research,Siruseri Biotech Park for Women,India.3Apollo Hospital and Research Foundation,India.4Transplant and General Surgery,American Samoa.5Department of Anesthesiology,Velammal Medical College Hospital& Research lnstitute,India.6Surgical Gastroenterology and Transplantation,Velammal Medical College Hospital&Research lnstitute,India.7Transplant science and ICU,MGM Health Care, India.8Institute of liver and multiorgan transplant, MGM Health Care, India.9Liver Transplant, Kauvery Hospitals, India.10Clinical Islet Cell Laboratory,Cardiovascular Innovation Institute,American Samoa.
Abstract Background: Diabetes is a widespread disease with increasing prevalence.Transplantation of islets of Langerhans is a viable treatment for a selected group of patients with repeated hypoglycemic episodes in type 1 diabetes.The countries where islet transplantation has not been explored suffer from insufficient knowledge concerning key elements of the isolation process.Donor and organ procurement parameters impact human islet yield, although for research purposes, islet yield may be secondary in importance to islet function.This paper will analyze the feasibility of research–only human islet isolation and signify parameters underlying a successful yield in the Indian population.This eventually can make islet transplantation a clinical reality in India. Method: After receiving the consent for procuring brain-dead pancreas from the first-degree of relatives, samples were collected and transported in a transportation buffer at 4 ℃.The procedure consists of a mechanically enhanced enzymatic digestion of the pancreas, after which it was taken for purification using Ficoll method, followed by islet quality testing. Results: Through 15 isolations done over a span of approximately 2 years during the COVID pandemic in India,we confirm that ischemic time and glycated hemoglobin, each have a negative impact on isolation purity and yield.Notably, extending cold ischemic tim beyond the typical clinical isolation cutoff of 12 hours (to ≥18 h) had a huge impact on islet function and yield.Age had a negative correlation with islet yield; however other biological parameters (specifically body mass index) and isolation variables appear to make a significant contribution to the heterogeneity of human islet yield.Our current work demonstrates the feasibility of extending acceptable cold ischemic time for research-focused human islet isolation and highlights the biological variation in isolation of human islets from donors with and without diabetes. Conclusion:India requires establishment of an islet transplant program using the current standard methods of“islet isolation” and donor program and process.Research should focus on improving standards in the islet preparation process to increase the number of successful preparations, shorten the isolation time, and increase patient safety so that the theoretical risk involved can become a practical reality.
Keywords: human islets; islet cell transplantation; type 1 diabetes mellitus; chronic pancreatitis; cold ischemia time; glycated hemoglobin; allo- and auto-transplantation
Introduction
Diabetes mellitus is rapidly on the rise and has been becoming one of the important threats to human health, causing a burden to society in this century [1].The global prevalence of diabetes is shifting significantly from developed countries to the developing countries.Histories of diabetes therapy include the discovery of insulin and successful methods of beta cell replacement, including whole pancreas and islet cell transplantation options [2].Oral anti-diabetic drugs and insulin administration are the standard forms of therapy, but these approaches do not mimic the pulsatile insulin secretory patterns of native β islets for the regulation of glucose in real-time nor provide tight control of blood glucose to avoid late complications of the disease.Transplantation of islet cells isolated from a donor pancreas has successfully controlled glucose levels in many countries.Islet cell transplantation is less invasive and more utopian as an approach.Also,while pancreas transplantation may not be suitable for all patients,islet cell transplantation can help many more people with different conditions [3].
The crucial role of the pancreas and islets of Langerhans in the development of diabetes was established in the late nineteenth century.Extensive studies on different animal models for over 50 years give hope of establishing a basis for human islet transplantation in unexplored countries[2].After the success of phase 3 clinical trials,and as it is already established in other parts of the country, we have the best chance to establish islet allo-transplantation as a treatment for type 1 diabetes and as an auto transplant, in case of chronic pancreatitis in India[4, 5].There are not many islet transplant centers in the world.Surprisingly, there are no islet transplant centers in the whole of Asia.However, we have currently initiated experimental research on the first 15 samples in India.Therefore, efforts must be made to increase the effectiveness of islet isolation and transplantation techniques.This will ensure establishing an islet transplantation program that can eventually be implemented as part of a routine in clinical practice.
Islet transplantation around the world
The success of the Edmonton protocol has spurred a wide widespread interest around the world.Shapiro et al.have proved improved glucose control in type 1 diabetic patients [5].The Government of Alberta, Canada and the University of British Columbia began funding islet transplants as a standard of care therapy [6].In Europe, many new centres were established and they followed Edmonton’s method[7–10].
The National Italian Transplant Centre and San Raffaele Scientific Institute, along with Niguarda Hospital are the two independent islet transplant programs in Italy [11].In 2018, Poland established their centres at the University of Warsaw and Medical University of Gdansk.Australia offers islet transplants to patients in a unique way called the national “spoke and wheel” program.This program offers islets to patients at a primary centre, but islets are isolated at one of several centers [12, 13].Considering the traditional values, Japan’s transplantation programs have been slowed down.National Health Services offer the islet program in Japan.It is interesting to note that the International center offers the islet program to patients under the National health schemes, either partially or on fully subsidized schemes[7, 8, 11, 12, 14–16].
Islet cell transplantation is categorized for brittle diabetes patients who lack the ability to secrete insulin.Considering the safety norms of islet transplantation and the least invasiveness in transplant procedures, remarkable progress has occurred in both the technical aspects of islet cell processing and the outcomes of clinical islet transplantation.This will be a technology that can offer a cure to hypoglycemic unawareness in type 1 diabetes mellitus (T1DM) and chronic pancreatitis [10].
Most of the pancreases in the country go unutilized if there is no need for therapeutic applications.In this situation, Indian research and government should work on the existing pancreas procurement program that provides for whole-pancreas transplantation to successfully establish the islet transplantation.These schemes should be under the State or Nations health so that even the poor patients are benefitted at the fullest.
This paper is aimed to bring “pancreatic islet transplantation” as a useful treatment option for patients with “brittle T1DM” and chronic pancreatitis by allo and autotransplantation.However, in India, this procedure is not even carried out as a part of experimental research initiatives.Therefore, efforts must be made to increase the effectiveness of islet isolation and transplantation techniques, thus ensuring implementation of islet transplantation as a part of routine clinical practice.
Method
Ethical approval for the organ procurement
Research involving humans, including observational, survey-based studies or any personal data, must have been performed by the declaration of Helsinki and must have been approved by an appropriate ethics committee and strictly abiding by this, the ethical committee of the present study was approved by Apollo Hospitals(AMH002-04/18) and Velammal Medical College and Hospital(VMCIEC/01-2021).The protocols were designed according to the guiding principles approved by the Indian Council of Medical Research without affecting the Indian organ procurement program.The primary importance was given to the transplant patients; if there were no takers for the organ, it was diverted for research.Human pancreata were obtained (with consent) from an adult heart-beating cadaver.Informed consent was specially sorted for the use of pancreatic tissue in research from Organ donors and all donors’families.
Donor selection
Donor pancreas quality is an important factor in successful islet isolation [17–20].However, pancreata are offered first for therapeutic application and then only for islet transplantation since whole-pancreas transplantation is considered an established treatment and islet research is considered experimental.We couldn’t fix any specific criteria on the selection of donors or pancreas,considering the organ procurement program and the Indian Council for Medical Research guidelines.
Pancreas retrieval
Fifteen human pancreata were retrieved following a protocol similar to that for whole-organ pancreas transplantation.En bloc dissection with hypothermic in situ vascular perfusion with University of Wisconsin solution along with immediate surface cooling of the pancreas was achieved with 4 ℃ice slush in the lesser omental sac[21–23].Surgeons took pancreas for biopsy-related studies and the remaining was given for the purpose of islet isolation.We couldn’t airlift the organs considering the present regulations and norms.Hence, the organs were transported with all necessary documents by road.After procurement, the pancreases were shipped in cold University of Wisconsin solution or histidine tryptophan ketoglutarate from the donor hospital to the islet isolation laboratory with cold ischemia time ranging between 4 hours 30 minutes and 19 hours 47 minutes.
Islet isolation
Our group has modified and developed an islet isolation protocol considering all the norms and regulations.This can be further adapted and modified to clinical protocol in a GMP (good manufacturing practices) facility.Extra fat, connective tissue and blood vessels were removed and the pancreas was washed in a cocktail of antibiotics that was weighed and dissected.A uniform mixture of exogenous enzymes,including collagenases and neutral proteases (Serva, GMP grade,Heidelberg, Germany), freshly dissolved in HBSS (Mediatech-Cellgro Inc., Manassas, VA, USA) was pre-warmed to 28–30 ℃ and the infusion of this blend of enzymes were done at 37 ℃.Infusion of enzymes usually distends the pancreas.Manual shaking in the Ricordi chamber where a solution containing the same enzyme blends circulates and disrupts pancreatic tissue[23, 24].
Pancreatic tissue samples were obtained every 5 to 10 minutes and the digestion process was observed.To evaluate the islets, the samples are suspended in a solution of HBSS containing dithizone, a dye that colors the islets red to distinguish them from unlabeled exocrine and ductal tissue [25, 26].When islets free of exocrine tissue are visible,enzyme activity is terminated by cooling and the addition of human serum albumin with HBSS.The samples were then centrifuged twice at 1200 rpm at 40 ℃for 5 minutes.The supernatant was discarded and the pellet was taken for purification using a discontinuous ficol gradient method.Depending on the pellet size, the gradient mixtures were prepared.The islet solution was mixed initially with the high-density gradient (1.119) and then slowly the medium and low-density gradients were layered carefully (1.083 and 1.077).It was then centrifuged at 2400 rpm for 20 minutes at 4 ℃.The islets were separated at the interphase.The islets were decanted into a fresh tube[27, 28].
Islet quantification and quality control testing
Islet yield is determined by direct count of the islets stained with dithizone [24, 27].An islet equivalent is equal to the volume of an islet with 150 μm diameters.Trypan blue exclusion assay was used to check the viability of islets.Samples of the islet cells as well as of the procurement fluid (the fluid in which the pancreas is preserved until isolation) are analyzed by Gram stain and sterility culture for microbiological contaminations.
Statistical analysis
All the statistical analysis was performed using Graph-pad prism(version 6).All the data were expressed as Mean ± standard deviation and Pearson correlation was done between the measured variables withP<0.05 was considered as statistically significant.
Results
Donor characteristics
Table 1 shows the donor characteristics of 15 islet isolations.The mean age of donors was 41 years and ranged from 18 to 76 years.Cerebrovascular accidents accounted for the most frequent causes of death.The mean CIT was 12 hours 39 minutes, ranging from 6 hours 40 minutes to 19 hours 47 minutes.The stay in the hospital for the majority of donors was less than 5 days.We have processed a total of 7 diabetic samples and 5 non-diabetic samples.The mean maximum and minimum body mass index (BMI) range from 33.1 to 17.9.The mean maximum and minimum glycated haemoglobin (HbA1c) were 8.3 and 5.2, respectively.
Islet processing details
Table 2 gives an idea about the islet processing details.Considering the regulatory norms as per the government and donor organ program, the sample weights vary every time.Hence, to present the results, we have considered the yield of islets per gram of tissue.The mean digestion times for all samples were between 25 to 30 minutes.The total number of viable cells per gram of the tissue for each sample is shown in Table 2.
There are numerous factors involved which will affect the isolation outcome.Digestion of the human pancreatic tissue and its separation from acinar tissue plays a prominent role.Based on our own human islet isolation experience, we have defined the following evaluative points during the isolation process.They are as follows: (1) The digestion time is different for each and every sample.(2) Once 50–60% of the islets are free and separated from acinar tissue, add dilution solution to cool the tissue; this plays a crucial role and the digestion process should be stopped.(3) During the washing, mixing and collection process,care must be taken to handle the tissues gently.(4) Once the digested mixture is ready, to enhance better purification results, it is always optimal to place the digested mixture of pancreatic tissue on ice for at least 30 minutes.
In Figure 1 and Figure 2, we can see a clear difference between the islets that were inside the tissue and the islets that were free.
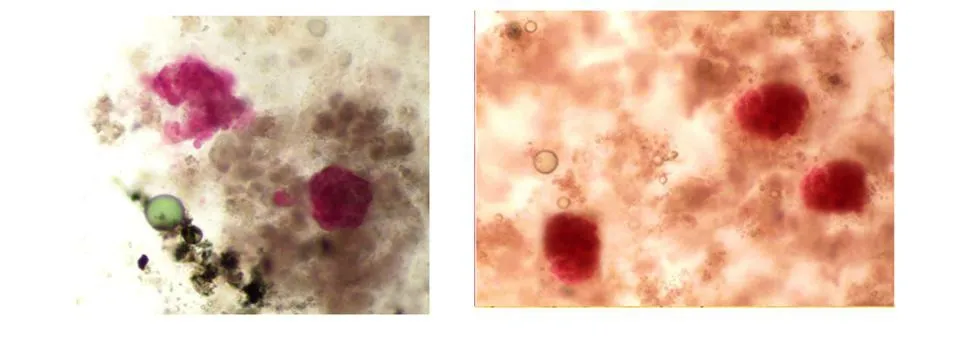
Figure 1 Microscopic image of human pancreatic islets stained with dithizone staining: islets seen inside the tissue after 15 mins of digestion

Figure 2 Microscopic image of human pancreatic islets stained with dithizone staining: islets seen separately after 25–30 mins of digestion
The following figures illustrate human pancreatic islets stained with dithizone staining.Islets are seen inside the tissue after 15 mins of digestion (Figure 1), islets are seen separately after 25–30mins of digestion (Figure 2) and individual islets are seen after purification(Figure 3).

Figure 3 Microscopic image of human pancreatic islets stained with dithizone staining: individual islets seen after purification
Correlation of the islet yield depending on the clinical parameters
It was interesting to note that the clinical parameters have a positive or negative influence over the islet yield.Our study found that cold ischemic time correlated positively with islet yield, whereas there was a negative correlation between HbA1c, age and islet yield.Again,there was a positive correlation between diabetic and non-diabetic patients along with BMI for the islet yield.Though there was a correlation, it was not statistically significant because of the smaller sample size(Table 2, Table 3).
Discussion
Our current study represents a comprehensive analysis of research-based islet products from a total of 15 isolations performed in the Indian population.Our short experience in the Indian population of isolating human islets suggests that many factors affect the ability to recover human islets.This paper aims to evaluate 15 consecutive human islet isolations and the variables were assessed for the multiorgan cadaveric donor and in the islet isolation process.
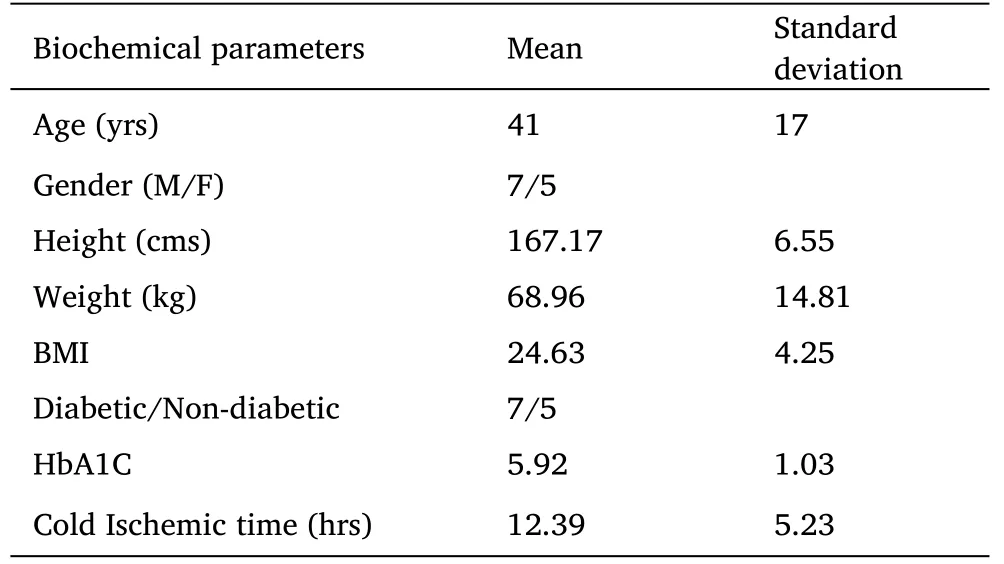
Table 1 Clinical and Biochemical characteristics of donors

Table 2 Islet processing details of Donor s
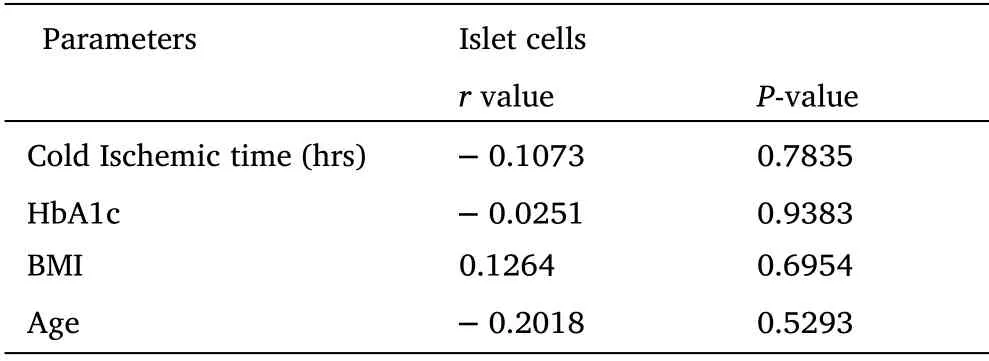
Table 3 Pearson correlation analysis of islet cells isolated with metabolic variables.
Basic and clinical research for diabetes revolves around human pancreatic islets as a valuable tissue resource.Reckard published the first report of this technique to yield successful glycemic control in rodents in 1973, followed by the first clinical report of successful islet transplantation in a patient with type 1 diabetes (T1D) mellitus by Najarian in 1977 [29, 30].A breakthrough to increase the yield and purity of islets was the invention of the Ricordi chamber in 1988,followed by Shapiro in the year 2000, which contributed to achieving better graft outcomes [31].Compared to other protocols, there was a huge success of the Edmonton protocol in T1D patients.Globally,different centers established islet transplantations, which have improved insulin independence rates to those of whole-pancreas-alone transplantations [32].
To the best of our knowledge, in Asia, especially India, there is a paucity of networking or coordinating efforts to facilitate the establishment of Islet transplant programs and distribution of human islets.Contributing reasons to this could be a lack of pancreas donors,a shortage in proper organ procurement programs possibly due to cultural and legislative rationale, and notably an insufficiency in resources allocated for the establishment and maintenance of human islet isolation infrastructure [33].Islet transplantation can be advantageous if translated to a clinical reality owing to its less-invasive procedure, low morbidity and technical ease in carrying out repeated transplantation of islets compared to pancreas transplantation.Though advantageous over pancreas transplantation,islet transplantation (both allo- and auto-transplantation) still remains an experimental process in India.This study can thus bring an optimistic change for countries that are yet to initiate the experimental procedures and establish the islet transplant program.
Our study has brought out multiple factors that can affect the quality of islet preparations (Table 1, Table 2).In accordance with other studies, we also observed donor characteristics to be a major factor influencing islet preparations' quality [34–37].Predictably,islet yield, purity, and bio potency were negatively impacted by high HbA1c levels or hyperglycemia[34].With regard to the donor’s age as a variable affecting the yield, purity and function of islets, there are controversial results.Few studies reported a negative impact, while one study stated a higher islet yield from pancreatic tissues of old-aged donors [34, 38, 39].There are also studies reporting no significant difference in the measured isolation outcome of islets between donors of old and young age.However, better graft functions after transplant were observed with young aged donors [40, 41].In these fifteen samples, age had a negative correlation with islet yield.Some studies observed a better yield of IEQs from donors having higher BMI [36, 37, 39].Lyon et al.correlated higher donor BMI with larger islet size but with either islet yield, purity or its function [34].Our study has inferred BMI to correlate positively with the islet yield.According to Wrenshall et al., pancreatic insulin content was positively correlated with increased body surface area [42].
Poor islet isolation outcome because of hyperglycemia has been ascertained in a number of donor variable studies; our study also observed the same.Poor isolation success can be because of post-stroke death and hyperglycemia resulting from perturbed hormonal control (catecholamines and cortisol) because of either an endogenous stress response or due to glucose-based intravenous solutions used during resuscitation [43].The most important reason for decreased isolation success can be hyperglycemis in the donor [43,44].Our study evaluated both the minimum and maximum HbA1c levels of our donors.And we could see that higher HbA1c levels resulted in giving islet yield, which was contradictory to the negative correlation observed in previous studies.Such inconsistencies with regard to donor characteristics are suggestive of other factors probably taking up a vital role in determining the isolation and graft outcomes of human islets.
Islet yield gets impacted by cold ischemia time (CIT) of the tissue.The CIT is the time period commencing from the time of procurement and preservation of the organ until it’s processed at the islet isolation facility [45].Though a CIT of less than 12 hours can be designated for clinical islet transplantation, it significantly restricts the sample count that can be accepted for transplantation, especially in areas where the nearest isolation facility is not in proximity [46, 47].Extending the pancreas CIT by up to 24 h moderately impacts the islet yield [34].In our study, CIT negatively correlated with islet yield; we excluded a few samples that had a longer CIT because of logistical reasons.We observed that extended CIT donor pancreas might remain suitable for islet isolation, especially for basic research.
The digestion of the pancreas predominantly influences islet quality; this crucial step is acknowledged widely as 'highly inconsistent in the process of human islet isolation [48–50].Poor islet yield and a variation in their quality can be a result of poor pancreas digestion.Substantial efforts are made to optimize enzymatic digestion [51, 52].Perhaps, enzyme blends are also highly variable due to differences between batches.
Ficoll-based density gradient centrifugation for Islet purification is the gold standard methodology that is widely employed for all basic research.The optiprep-based density gradient purification method can be used to reduce the production of cytokines/chemokines from islet preparations and improve the survival of beta cells [53, 54].Downsizing the inconsistencies and inefficiencies of islet isolation procedures will sustainably benefit the community and equally facilitate islet transplantation and research activities.The data that is presented in this study is just an example to bring awareness to clinicians, basic science investigators, policymakers and organ coordinators of the country who determine the availability of donors and implement this in clinical practice.Increased sample size and further research is the need of the hour to make this data more viable.
Establishment of an effective organ donor program in India would pave the way for islet transplantation being set up on the strength of an existing pancreas procurement program, which provides for whole-pancreas transplantation.We strongly believe that achieving good-quality human islet isolation strongly relies on local organ donor procurement programs.Local donation significantly reduces hypothermic cold storage time that elapses even before the pancreas is subjected to islet isolation, thus optimizing the separation of islets from the pancreatic exocrine and ductal cells.
Conclusion
Islet transplantation can become a promising, cutting-edge therapy for treating patients with T1DM and chronic pancreatitis.For successful clinical islet transplantation, many obstacles must be overcome so that it can become a reality in the near future.
We would like to highlight some of the major obstacles, which restrict countries like India from bringing islet transplantation as standard therapy for T1D and chronic pancreatitis.(1) Organs from deceased donors become available every year but only a few are used for whole organ pancreas transplantation and the rest of the pancreas are discarded as there is a paucity in the law system to use law for the purpose of islet transplantation.(2) Shortage of islets considering the diabetic load in the country.
It will be a great initiative if appropriate laws are implemented to facilitate the accessibility of the organ (pancreas) for transplantation and further islet research.In India, a local, multiorgan donor pancreas procurement program can generate an optimized source of purified viable islets for transplantation into patients with T1DM receiving the best medical therapy.
- Life Research的其它文章
- Exploring the practice of common oral diseases among the patients visiting in the selected dental college and hospital in Bangladesh
- Different levels of MUC5AC and MUC5B genes expression in severe allergic versus non-allergic asthma
- Research progress on iron homeostasis regulation and heart-related diseases
- The regulatory variant rs17612742 confers the risk of large artery atherosclerotic stroke by increasing the expression of endothelin receptor type A
- Physiological signal processing in heart rate variability measurement: A focus on spectral analysis
- Research status of persistent vegetative state in recent 20 years: A bibliometric analysis

