Short- and long-term results of open vs laparoscopic multisegmental resection and anastomosis for synchronous colorectal cancer located in separate segments
Ji-Chuan Quan, Xin-Jun Zhou, Shi-Wen Mei, Jun-Guang Liu, Wen-Long Qiu, Jin-Zhu Zhang, Bo Li, Yue-Gang Li, Xi-Shan Wang, Hu Chang, Jian-Qiang Tang
Abstract
Key Words: Synchronous colorectal cancer; Separate segments; Laparoscopic surgery; Multisegmental resection; Short-term efficacy; Prognosis
INTRODUCTION
Synchronous colorectal cancer (SCRC), a colorectal malignancy, refers to the simultaneous presence of multiple primary colorectal cancers (CRCs) in one patient. SCRC lesions can be located in the same segments, adjacent segments, or different segments of the colorectum. For patients with SCRC localized in separate segments, multisegmental resection and anastomosis are often selected for treatment. Compared to conventional surgery, multisegmental resection is less common and more difficult. Selection of the optimal surgical method to promote rapid recovery in patients with SCRC involving separate segments still requires further study.
Previous studies have shown the safety and advantages of laparoscopic surgery in treating solitary CRC[1-5]. However, to date, there are few comparisons of the application of laparoscopic multisegmental resection and anastomosis (LMRA) and open multisegmental resection and anastomosis (OMRA) for SCRC. Therefore, the safety and efficacy of LMRA are not adequately understood and require further evaluation.
To determine the efficacy and safety of LMRA in patients with SCRC involving separate segments, a retrospective twoinstitution investigation was performed to compare the short-term surgical results, 5-year overall survival (OS) rate, as well as the 5-year disease-free survival (DFS) rate of patients receiving LMRA and OMRA.
MATERIALS AND METHODS
Selection of patients
Patients with SCRC who underwent surgery between January 2010 and December 2021 at the Cancer Hospital, Chinese Academy of Medical Sciences and the Peking University First Hospital were included. Multiple CRC lesions were diagnosed following published guidelines[6].
The following types of patients were included: (1) SCRC patients with pathological confirmation of lesions as primary adenocarcinoma; (2) SCRC patients with one lesion in the right hemicolon and the others located in the sigmoid colon or rectum; and (3) patients receiving right hemicolectomy as well as anterior resection of the rectum or right hemicolectomy and sigmoid colectomy. The following categories of patients were excluded: (1) Those with familial adenomatous polyposis, ulcerative colitis, hereditary nonpolyposis CRC, or Lynch syndrome; (2) patients with SCRC involving the same segment; (3) patients with SCRC involving adjacent segments; (4) those receiving Hartmann’s procedure or abdominal perineal resection; (5) those receiving subtotal colectomy, total colectomy, or proctocolectomy with ileoanal anastomosis; and (6) SCRC patients with distant metastasis. The selected patients were included in the LMRA and OMRA groups based on the surgical method. The study was approved by the Ethics Committee of Cancer Hospital, Chinese Academy of Medical Sciences.
Data collection
The following clinicopathological data were collected: Age, gender, abdominal surgery history, concomitant diseases, preoperative chemotherapy, carbohydrate antigen 19-9 (CA19-9) level, carcinoembryonic antigen (CEA) level, American Society of Anesthesiologists (ASA) physical status level, surgical approach (laparoscopic or open), operative time, volume of blood loss (mL), postoperative first exhaust time (d), time to first liquid diet (d), postoperative hospital stay (d), postoperative complications, classification of complications, tumor size (cm), tumor differentiation status, N stage, T stage and TNM stage, total number of positive lymph nodes (LNs), and number of LNs dissected. Pathological staging was evaluated using the American Joint Committee on Cancer (8thed.) staging system. The Clavien-Dindo (CD) system[7] was employed to grade postoperative complications.
Follow-up
Patients were followed up through telephone calls or outpatient examination. The following time frame was chosen: every 3 mo in the first 2 years following surgery, every 6 mo at 3–5 years following surgery, and then yearly 5 years after surgery. Follow-up assessment included physical examination, determination of serum tumor marker levels, CT scans of the abdomen, chest, and pelvic area, and colonoscopy.
Statistical analysis
The Mann-WhitneyUtest or Student’st-test was used to compare continuous variables; Fisher’s exact test or the chisquare test was used to compare categorical variables. The Kaplan-Meier analysis was employed to create survival curves. Survival differences were compared between the groups by the log-rank test. The Cox proportional hazards model was used to conduct univariate and multivariate prognostic analyses. A value ofP< 0.05 was considered statistically significant. Statistical Product and Service Solutions (SPSS) version 26.0 from IBM (Armonk, NY, United States) was used for statistical determinations.
RESULTS
Clinicopathological characteristics
From January 2010 to December 2021, 605 SCRC patients underwent surgical treatment at the above-mentioned institutions. Of these 605 patients, 496 patients were excluded according to the aforementioned criteria. Finally, 109 patients with SCRC located in separate segments were included, with 41 and 68 patients placed in the OMRA and LMRA groups, respectively.
Clinicopathological characteristics of the patients are shown in Table 1. As noted in this table, the groups did not differ significantly in age, gender, abdominal surgery history, concomitant diseases, preoperative chemotherapy, CA19-9 and CEA levels, ASA class, postoperative chemotherapy, tumor size, tumor differentiation status, N stage, T stage, and TNM stage.
Surgical results
Table 2 presents the surgical outcomes of both groups. LMRA patients showed markedly less intraoperative blood loss than OMRA patients (100vs200 mL,P= 0.006). The LMRA group showed a significantly shorter postoperative first exhaust time (2vs3 d,P= 0.001), postoperative first fluid intake time (3vs4 d,P= 0.012), and postoperative hospital stay (9vs12 d,P= 0.002) than the OMRA group. The incidence of total postoperative complications (CD grade ≥ II) was 2.9% in the LMRA group; this percentage was markedly lower than the value (17.1%) recorded for the OMRA group (P= 0.025). Furthermore, LMRA patients had a lower incidence of anastomotic leakage than OMRA patients; however, the difference was nonsignificant (2.9%vs7.3%,P= 0.558). The mean number of LNs dissected was significantly greater in LMRA patients as compared to OMRA patients (45.2vs37.3,P= 0.020). However, there were no significant differences in operating time, mortality rate, and number of positive LNs between the two groups.
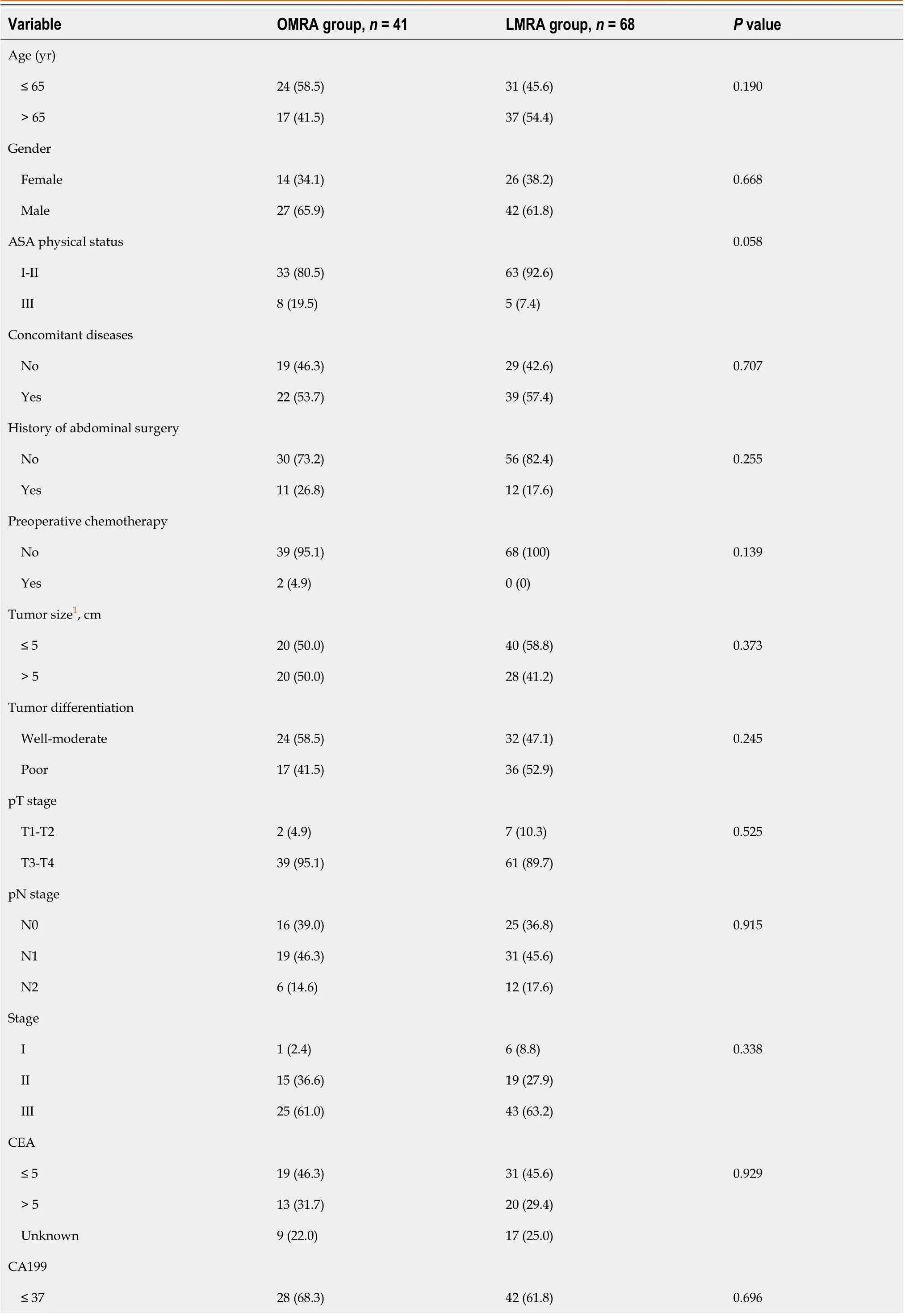
Table 1 Basic characteristics between laparoscopic group and open group, n (%)

1Unknown for one patient.OMRA: Open multisegmental resection and anastomosis; LMRA: Laparoscopic multisegmental resection and anastomosis; CA19-9: Carbohydrate antigen 19-9; CEA: Carcinoembryonic antigen; ASA: American Society of Anesthesiologists.
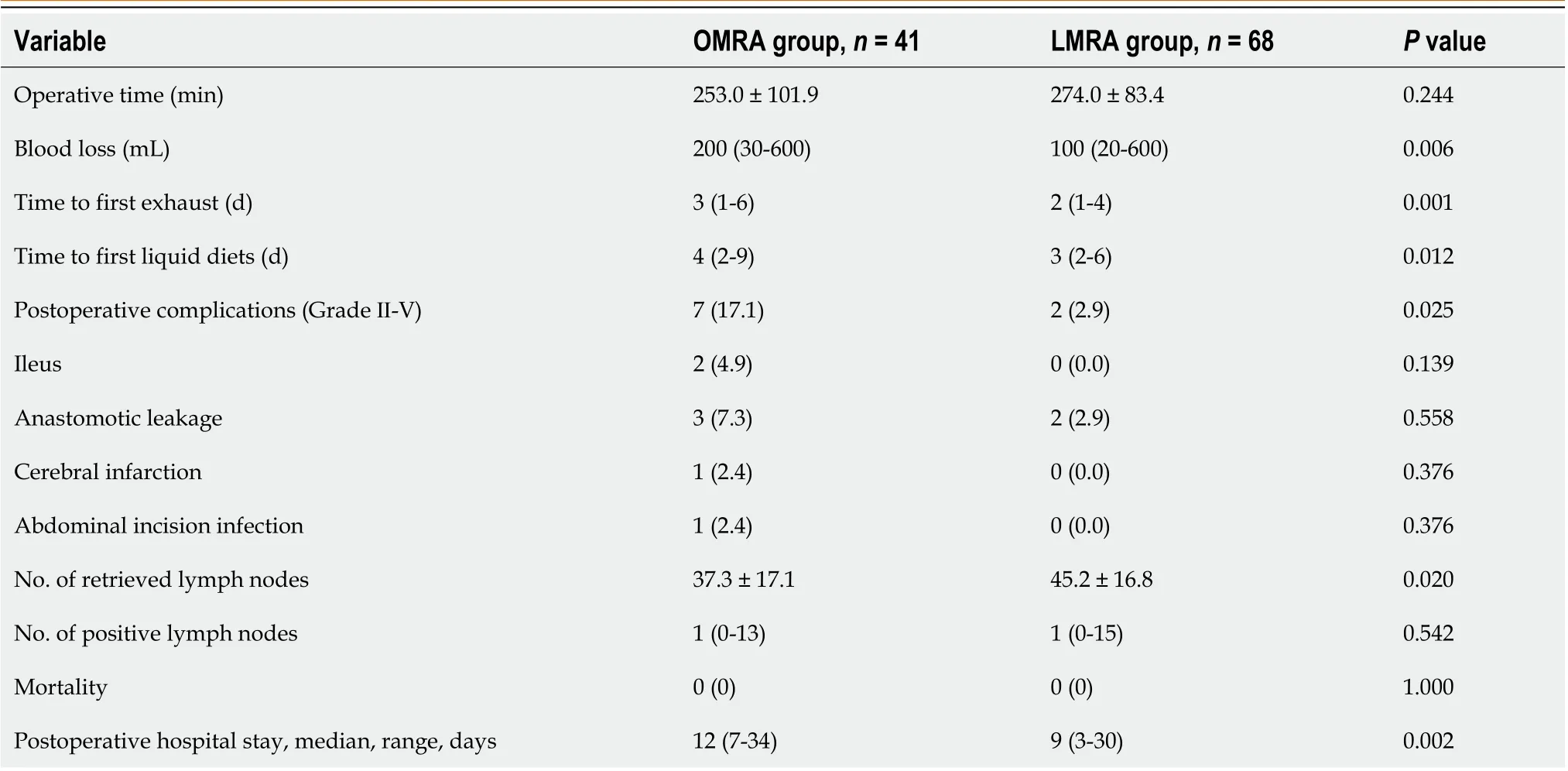
Table 2 Surgical results between laparoscopic group and open group
Long-term oncological consequences
The median follow-up period was 53.5 mo for all patients. OMRA patients had 3-year and 5-year OS rates of 87.5% and 82.9%, respectively; these rates for LMRA patients were 84% and 78.2%, respectively. Additionally, the 3-year and 5-year DFS rates for OMRA patients were 82.6% and 78.3%, respectively; these rates for LMRA patients were 79.3% and 72.8%, respectively. Both groups showed no significant differences in OS (P= 0.690) and DFS (P= 0.694) rates (Figure 1). According to the multivariate prognostic analysis, N stage was an independent prognostic factor for OS [hazard ratio (HR) = 10.161,P= 0.026] and DFS (HR = 13.017,P= 0.013) (Table 3).
DISCUSSION
SCRC involving separate segments is a relatively rare type of CRC. Surgeons can choose two regional resections and anastomoses for preserving the left hemicolon or extensive resection, for example, total colectomy, subtotal colectomy, or proctocolectomy with ileoanal anastomosis. Which is the best treatment option is still unresolved. Leeet al[8] retrospectively analyzed the postoperative bowel movements in SCRC, and found that the mean number of bowel movements in a two regional resections group and an extensive resection group was 1.9 times and 4.3 times, respectively, with a significant difference between the two groups. Youet al[9] compared the bowel function and quality of life between patients with extended resections and segmental colonic resections. The results showed that median daily stool frequency after segmental resections, ileosigmoid anastomosis and ileorectal anastomosis was 2, 4 and 5, respectively, and the overall quality of life was 98.5, 94.9, and 91.2, respectively. As multisegmental resection provides better postoperative defecation function and quality of life[8,9] and does not increase complications such as anastomotic leakage[9], this technique is recommended by some researchers.
Following advances in laparoscopic techniques, several studies have confirmed that laparoscopic radical resection of CRC is safe and reliable; moreover, it can achieve the same curative effect as open surgery[10-14] and offers the advantages of minimally invasive surgery, such as small incision, mild postoperative pain, and rapid recovery[15,16]. However, unlike conventional CRC surgery, surgical treatment of SCRC with multisegmental resection is more difficult as more anastomoses are required. Presently, there are limited reports on the differences between laparoscopic and open surgical approach for SCRC involving separate segments. These studies are limited to single-center investigations with few patients and are mainly focused on the analysis of short-term efficacy; consequently, they lack a comparison of longterm prognosis[17,18]. Here, we studied patients from two institutions with SCRC located in separate segments. These patients underwent either LMRA or OMRA as curative surgery. We found that intraoperative blood loss together with postoperative parameters such as postoperative first exhaust time, postoperative first fluid intake time, the incidence of postoperative complications, and postoperative hospital stay were less in LMRA patients when compared with those in OMRA patients. Furthermore, LMRA patients had more LNs dissected than OMRA patients, while the prognosis for both groups was similar. To our knowledge, this study includes the largest sample size for comparing LMRA and OMRA approaches with regard to short-term efficacy as well as long-term results.
Intraoperative blood loss and the incidence of postoperative complications are critical parameters for evaluating whether a surgical procedure is safe. Previous studies have confirmed that laparoscopic surgery has more advantages than open surgery for solitary CRC in terms of less intraoperative blood loss[19-22], reduced postoperative oral intake time[21,22], and shorter postoperative hospital stay[21-25]. Moreover, previous single-center, small-sample studies have reached the same conclusion for patients with SCRC involving different segments. Takatsuet al[17] compared the shortterm efficacy of LMRA and OMRA in 42 patients with SCRC located in different segments; the authors noted that postoperative hospital stay and intraoperative blood loss were significantly decreased in the laparoscopic group as compared to the open surgery group. Nozawaet al[18] performed a single-center study of 25 patients with SCRC; the authors found that the laparoscopic group showed less intraoperative blood loss than the open surgery group. Here, we analyzed the surgical results of 109 patients with SCRC located in separate segments and found significantly less intraoperative blood loss in LMRA patients than in OMRA patients. Moreover, the total postoperative complication as well as hospital stay were remarkably better in LMRA patients. Furthermore, the operating time was not significantly increased in LMRA patients.
The number of dissected LNs is another crucial factor in evaluating radical surgery of CRC. In accordance with the guidelines of the National Comprehensive Cancer Network, the number of dissected LNs should be 12 or more after radical surgery of CRC. If the number of dissected LNs is small, the final staging will be affected. For SCRC located in separate segments, the number of dissected LNs is another vital indicator in evaluating surgical quality. Laparoscopy enables magnification of the operative field; hence, the dissection of LNs by laparoscopy is more precise than that by open surgery. A significantly higher number of LNs have been dissected by laparoscopy than by traditional open surgery[17]. The present study revealed that the average number of LNs dissected in LMRA patients was significantly more than that in OMRA patients; this finding was in agreement with the result of Takatsuet al[17]. However, both groups did not significantly differ in the number of positive LNs.
According to several studies, both laparoscopic and open surgeries have similar oncological results[26-30]. However, for SCRC located in separate segments, comparative studies on the long-term efficacy of LMRA and OMRA are presently inadequate. In our study, the 5-year OS rates of LMRA and OMRA patients were 78.2% and 82.9%, respectively, while the 5-year DFS rates of LMRA and OMRA patients were 72.8% and 78.3%, respectively. Both groups did not markedly differ in long-term prognosis. We further performed a multivariate prognostic analysis and found that the N stage was the sole independent prognostic factor that affected DFS and OS.
There are a few limitations in this research. First, selection bias probably existed due to the study’s retrospective nature. Second, some patients’ clinical data were incomplete, such as the time of first ambulation and postoperative pain score; thus, we could not compare and analyze the differences between open and laparoscopic approaches with regard to these aspects. Third, as the incidence of SCRC located in separate segments is low, although the sample size in this study is the largest thus far, the number of patients included in the analysis is still small. Therefore, multicenter prospective studies are needed in the future to confirm the advantages of LMRA.
CONCLUSION
LMRA is safe and feasible for SCRC located in separate segments; moreover, it has the benefits of less bleeding, rapid recovery, shorter postoperative hospital stay, reduced complications, a greater total number of LNs dissected and achieves the same long-term oncological outcomes as OMRA.
ARTICLE HIGHLIGHTS


Research results
LMRA patients showed significantly shorter postoperative first exhaust time, postoperative first fluid intake time, and postoperative hospital stay than OMRA patients. Intraoperative blood loss, and the incidence of total postoperative complications (Clavien-Dindo grade: ≥ II) were markedly less in the LMRA group. The mean number of lymph nodes dissected was significantly higher in the LMRA group. Prognostic analysis showed that N stage was the independent prognostic factor for overall survival and disease-free survival.
Research conclusions
On the basis of this study, we conclude that LMRA has some short-term advantages compared with OMRA, and is safe and feasible for patients with SCRC located in separate segments.
Research perspectives
Future multicenter prospective studies are needed to further confirm the advantages of LMRA.
FOOTNOTES
Author contributions:Quan JC and Zhou XJ contributed equally to this work; Quan JC and Chang H wrote the manuscript; Tang JQ, Zhou XJ and Wang XS conceived and designed the study; Quan JC, Liu JG, Chang H, Mei SW and Zhou XJ collected the data; Zhang JZ, Qiu WL, Li B and Li YG analyzed the data; all authors made critical revisions for the manuscript and approved the final manuscript.
Institutional review board statement:This study was approved by the Ethics Committee of Cancer Hospital, Chinese Academy of Medical Sciences.
Informed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:The authors declare no conflict of interest.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Ji-Chuan Quan 0000-0002-4250-3699; Xin-Jun Zhou 0009-0003-5479-1733; Shi-Wen Mei 0000-0002-9735-3261; Jun-Guang Liu 0000-0001-5230-4565; Wen-Long Qiu 0000-0002-6938-7878; Jin-Zhu Zhang 0000-0001-6979-0539; Bo Li 0000-0001-6763-230X; Yue-Gang Li 0000-0001-9115-3448; Xi-Shan Wang 0000-0002-1675-5083; Hu Chang 0009-0009-8157-1182; Jian-Qiang Tang 0000-0003-3933-8060.
S-Editor:Yan JP
L-Editor:A
P-Editor:Yan JP
 World Journal of Gastrointestinal Surgery2023年9期
World Journal of Gastrointestinal Surgery2023年9期
- World Journal of Gastrointestinal Surgery的其它文章
- Preoperative and postoperative complications as risk factors for delayed gastric emptying following pancreaticoduodenectomy: A single-center retrospective study
- Comparative detection of syndecan-2 methylation in preoperative and postoperative stool DNA in patients with colorectal cancer
- Preoperative prediction of microvascular invasion in hepatocellular carcinoma using ultrasound features including elasticity
- Surgical management of gallstone ileus after one anastomosis gastric bypass: A case report
- Hepatic ischemia-reperfusion syndrome and its effect on the cardiovascular system: The role of treprostinil, a synthetic prostacyclin analog
- Advances and challenges of gastrostomy insertion in children
