Global burden of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease,1990-2019
Zhi-Peng Liu,Guo-Qing Ouyang,Guo-Zhen Huang,Jie Wei,Luo Dai,Song-Qing He,Guan-Dou Yuan
Abstract BACKGROUND Nonalcoholic fatty liver disease (NAFLD) has become the leading cause of cirrhosis and other chronic liver diseases (COCLDs).AIM To conduct a comprehensive and comparable updated analysis of the global,regional,and national burden of COCLDs due to NAFLD in 204 countries and territories from 1990 and 2019 by age,sex,and sociodemographic index.METHODS Data on COCLDs due to NAFLD were collected from the Global Burden of Diseases,Injuries,and Risk Factors Study 2019.Numbers and age-standardized prevalence,death,and disability-adjusted life years (DALYs) were estimated through a systematic analysis of modelled data from the Global Burden of Diseases,Injuries,and Risk Factors Study 2019.The estimated annual percentage change was used to determine the burden trend.RESULTS In 2019,the global age-standardized prevalence rate of COCLDs due to NAFLD was 15022.90 per 100000 population [95% uncertainty interval (UI): 13493.19-16764.24],which increased by 24.51% (22.63% to 26.08%) from 1990,with an estimated annual percentage change of 0.78 (95% confidence interval: 0.74-0.82).In the same year,however,the age-standardized death rate and age-standardized DALYs per 100000 population were 1.66 (95%UI: 1.20-2.17) and 43.69 (95%UI:31.28-58.38),respectively.North Africa and the Middle East had the highest prevalence rates of COCLDs due to NAFLD.The death rate increased with age up to the 95+age group for both sexes.Males had higher numbers of prevalence,death rate,and DALYs than females across all age groups before the 65-69 age group.The sociodemographic index was negatively correlated with the age-standardized DALYs.CONCLUSION Globally,the age-standardized prevalence rate has increased during the past three decades.However,the agestandardized death rate and age-standardized DALYs decreased.There is geographical variation in the burden of COCLDs due to NAFLD.It is strongly recommended to improve the data quality of COCLDs due to NAFLD across all countries and regions to facilitate better monitoring of the burden of COCLDs due to NAFLD.
Key Words: Cirrhosis;Nonalcoholic fatty liver disease;Global burden of disease;Prevalence;Disability-adjusted life years;Death
INTRODUCTION
The incidence and prevalence of nonalcoholic fatty liver disease (NAFLD) have been rapidly increasing worldwide over the past few decades.Recent estimates suggest that approximately 25% of the world’s population is affected by NAFLD,with projections indicating a potential 56% surge in the prevalence of nonalcoholic steatohepatitis (NASH) within the coming decade[1].NAFLD encompasses a spectrum of liver damage,ranging from simple steatosis to NASH,fibrosis,cirrhosis,and even hepatocellular carcinoma[2].It is noteworthy that NAFLD now stands as the fifth leading cause of mortality among young adults within the category of metabolic diseases.Alarming forecasts predict a staggering 158.4%increase in its death rate by the year 2050[3].Conversely,another separate study demonstrated divergent trends,finding that the age-standardized prevalence rate (ASPR) of NAFLD increased while the age-standardized death rate (ASDR) and age-standardized disability-adjusted life-year (DALY) rate (ASDAR) decreased from 1990 to 2019[4].
Cirrhosis is the leading cause of liver-related morbidity,contributing to more than 1 million deaths annually worldwide.The mortality increase escalates markedly for individuals grappling with decompensated cirrhosis[5],and the deaths from cirrhosis increased by 47.15% globally from 1990 to 2017[6].Beyond mortality statistics,cirrhosis imposes a significant public health burden globally,substantially compromising quality of life[7,8].The etiologies of cirrhosis include alcoholic liver disease,hepatitis B virus,hepatitis C virus,and NAFLD[9,10].Over the past few decades,universal hepatitis B virus vaccination initiatives,coupled with rising obesity rates and the prevalence of type 2 diabetes,have positioned NAFLD as a major etiological factor contributing to cirrhosis[11-14].
Chronic liver disease (CLD) is a disease that is characterized by decreased liver function resulting from chronic inflammation or injury to the liver,leading to fibrosis and cirrhosis that progresses for more than 6 mo[15,16].This spectrum encompasses an array of liver pathologies,encompassing inflammation,cirrhosis,portal hypertension,and hepatorenal syndrome.Notably,the incidence of CLD is increasing yearly,and it is now the fifth leading cause of death in the United Kingdom.In Western regions,NAFLD has become the leading cause of CLD[17].Today,the United States has nearly 4.5 million adults afflicted by cirrhosis and CLD,resulting in an overall death toll of 414731[16].However,no studies have focused on the epidemiology of cirrhosis and other CLDs (COCLDs) due to NAFLD across the globe.
In the Global Burden of Diseases,Injuries,and Risk Factors Study (GBD) 2017,it was shown that the incidence of cases of liver cirrhosis caused by NASH increased by approximately 105.56%,and the age-standardized incidence rate increased by 1.35%.This study only included data from 195 countries,and data on prevalence,death,and DALYs were not provided[18].Furthermore,no updated global studies on COCLDs due to NAFLD have been published since the 2017 estimates.Using the data from the GBD 2019,we conducted this comprehensive,updated analysis of the global,regional,and national levels of prevalence,death rate,and DALYs of COCLDs due to NAFLD with regard to age-standardized rates (ASRs) and raw numbers from 1990 to 2019,stratified by sex,age,and sociodemographic index (SDI).
MATERIALS AND METHODS
Overview
The GBD 2019 was conducted by the Institute of Health Metrics and Evaluation and analyzed approximately 369 diseases and injuries,282 causes of death,and 84 risk factors from 204 countries/territories,21 regions,and 7 superregions from 1990 to 2019[19].Detailed methods for GBD 2019 regarding date inputs,analytical processes,and outputs have been described in previous publications[19,20].Additional information on fatal and nonfatal estimates can be found at https://vizhub.healthdata.org/gbd-compare/ and http://ghdx.healthdata.org/gbd-results-tool.Our study complied with the Guidelines for Accurate and Transparent Health Estimates Reporting statement[21].
Case definition and data sources
NAFLD was defined as a range of liver conditions that mimic alcoholic liver disease but occur in people who drink little to no alcohol.It includes nonalcoholic fatty liver (characterized by fat deposition in liver cells),NASH (characterized by fat deposition and inflammation),and cirrhosis[19].Cirrhosis is a CLD in which there is progressive destruction of functional hepatic cells and replacement with fibrosis (scarring) of the liver.In GBD 2019,COCLDs due to NAFLD were defined as COCLDs that were specifically caused by NAFLD,excluding all other potential etiologies[19].All the GBD data used in this study are publicly available online at the Global Health Data Exchange.
Data processing and disease modelling
The Bayesian meta-regression tool DisMod-MR 2.1 was used to assess and model estimates of the burden of COCLDs due to NAFLD by pooling all the available epidemiological data.Prior settings included remission of 0 before the age of 15 years in the DisMod-MR 2.1 model.No prevalence of COCLDs due to NAFLD before the age of 15 years was assumed.The age range was restricted to ≥ 15 years and was divided into 17 5-year age groups.
The estimated annual percentage change (EAPC) values were calculated to reflect the change in ASRs over a specified period.EAPC values above or below 0 indicate that the ASR is increasing or decreasing,respectively.If the EAPC range includes 0,this means the ASR is stable during this period.ASPR,ASDR,ASDAR,and EAPC were used to quantify global trends of COCLDs due to NAFLD.
The SDI was used as a composite indicator of the development status in each country and territory.It was calculated based on lag-distributed income,the total fertility rate for individuals younger than 25 years,and average years of education in people older than 15 years.SDI ranged from 0 to 1,with a higher score indicating a higher level of development.The 204 countries and territories were categorized into five groups: low SDI,low-middle SDI,middle SDI,high-middle SDI,and high SDI.
Statistical analyses
Smoothing spline models were employed to examine the shape of the correlation curve between the burden index of COCLDs due to NAFLD and SDI according to the GBD estimates across 204 countries and 21 regions from 1990 to 2019.The 95% uncertainty intervals (UIs) were defined as the 2.5 to the 97.5 percentile of the ordered draws.R software version 3.6.3 was used for all statistical analyses and figures.APvalue of < 0.05 was considered statistically significant.
RESULTS
Global level
Globally in 2019 there were 1235652879 (95%UI,1109501987-1378481210) prevalent cases of COCLDs due to NAFLD.From 1990 to 2019,the global ASPR increased from 12065.15 (10779.06-13536.49) to 15022.90 (13493.19-16764.24) per 100000 population,with an EAPC of 0.78 (0.74-0.82) (Table 1,Figure 1).COCLDs due to NAFLD accounted for 134240(96483-176920) deaths globally in 2019,which was a substantial increase of 76.73% (61.23%-94.75%) over that in 1990.The ASDR of COCLDs due to NAFLD decreased from 1.94 per 100000 population (1.39-2.59 per 100000) in 1990 to 1.66 per 100000 population (1.20-2.17 per 100000) in 2019,with an EAPC of 0.65 (-3.68-2.48) (Table 1,Supplementary Figure 1).In the same year,COCLDs due to NAFLD accounted for 3621471.92 (2585375.27-4862918.36) DALY cases at the global level with an ASR of 43.69 per 100000 population.The global ASDAR was reduced from 51.92 per 100000 population (37.23-69.19 per 100000) in 1990 to 43.69 per 100000 population (95%UI: 31.28-58.38) in 2019,with an EAPC of -0.73 (-1.33 to -0.13) (Table 1,Supplementary Figure 2).
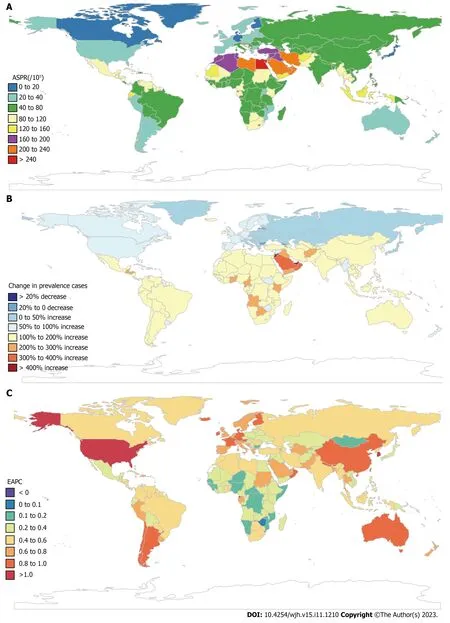
Figure 1 Global disease burden of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease by countries and territories for both sexes combined.A: The age-standardized prevalence rate (ASPR) of cirrhosis and other chronic liver diseases (COCLDs) due to nonalcoholic fatty liver disease (NAFLD) in 2019;B: The percentage change in prevalence cases of COCLDs due to NAFLD between 1990 and 2019;C: The estimated annual percentage change of COCLDs due to NAFLD ASPR from 1990 to 2019.EAPC: Estimated annual percentage change.
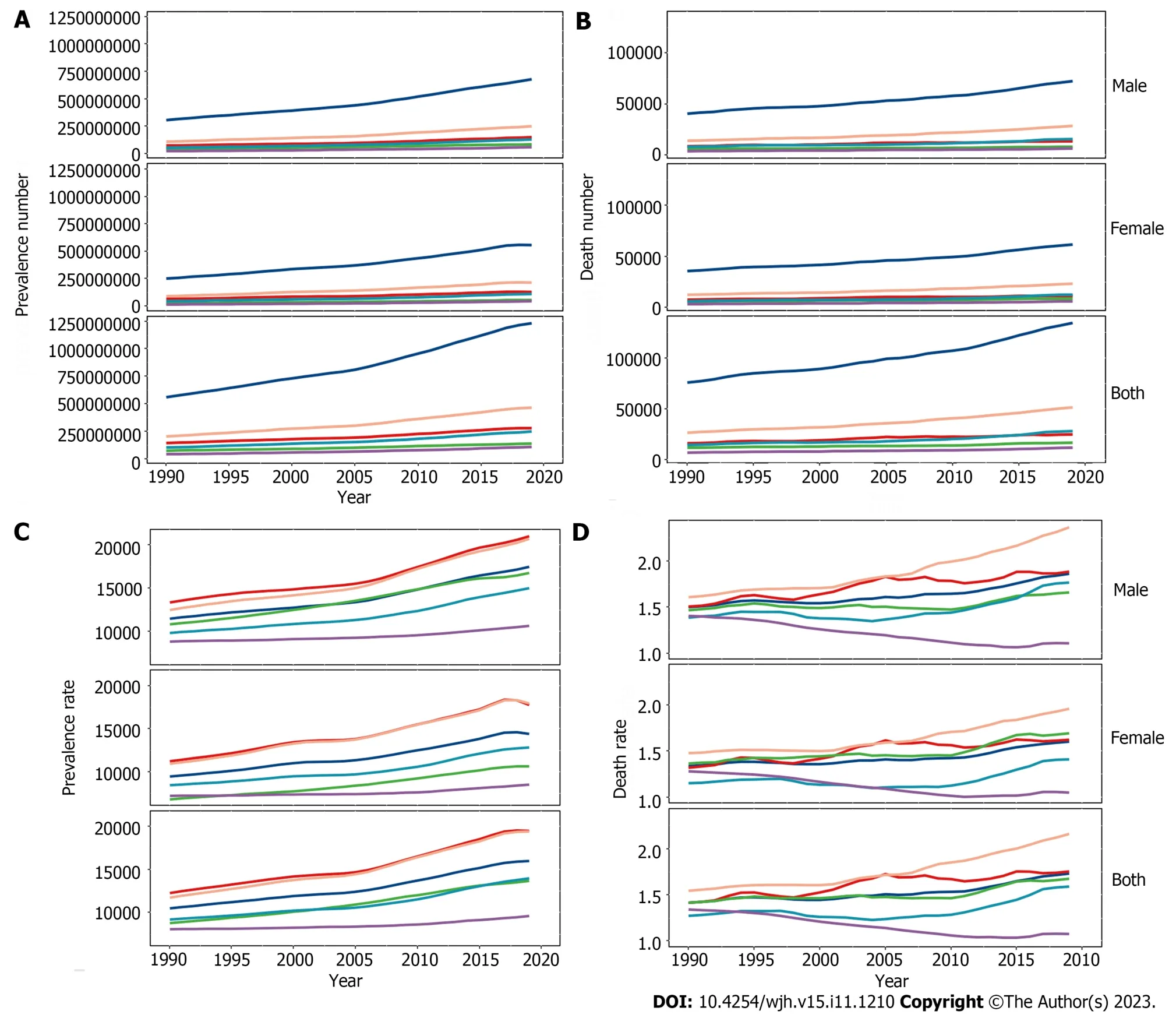
Figure 2 Cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease at the global and regional levels from 1990 to 2019. A: Prevalence number;B: Death number;C: All-age prevalence rate;D: All-age death rate.
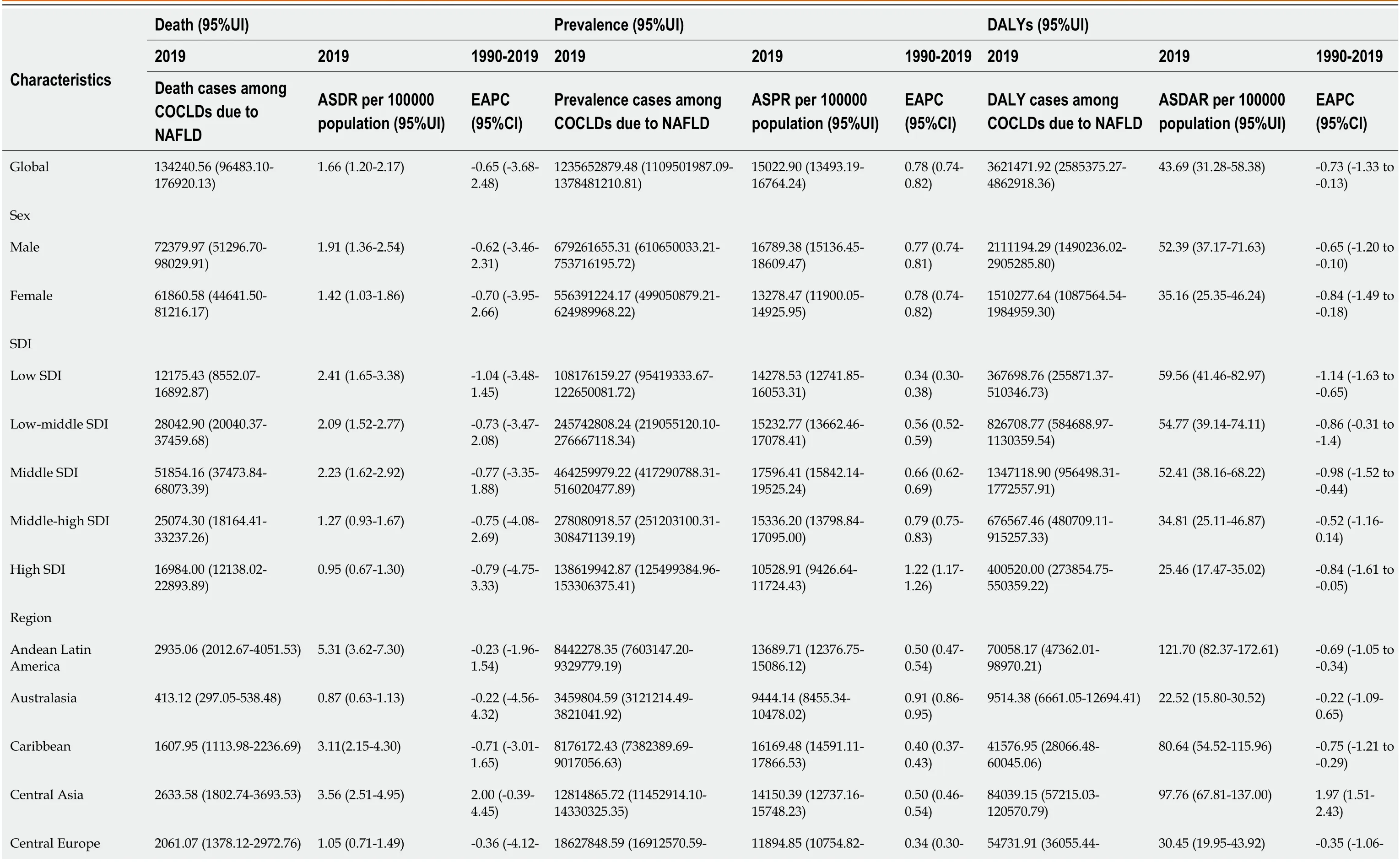
Table 1 Global burden of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease in 204 countries and territories from 1990 to 2019
SDI regions and 21 GBD region levels
The number of prevalence,deaths,and DALYs of COCLDs due to NAFLD increased in all five SDI regions from 1990 to 2019.Among them,the greatest increases in prevalence (1.54-fold),deaths (0.96-fold),and DALY (0.77-fold) cases were observed in low-SDI,middle-SDI,and low-middle-SDI regions,respectively (Figure 2,Supplementary Figure 3).All-age prevalence rates of COCLDs due to NAFLD increased across all SDI quintiles,with the most significant increase observed in the middle-SDI region (0.65-fold).Outside of the low-SDI quintile,all-age death rates and DALYs showed an increasing trend.The ASDR and ASDAR of COCLDs due to NAFLD exhibited a decreasing trend across all five SDI quintiles.The low-SDI quintile had the greatest absolute decreases in the ASDR (EAPC=-1.04;-3.48-1.45) and the ASDAR (EAPC=-1.14;-1.63 to -0.65).The ASPR of COCLDs due to NAFLD increased in all SDI regions from 1990 to 2019,with the highest increase observed in the high-SDI region (EAPC=1.22;1.17-1.26) (Table 1,Supplemen-tary Figure 4).
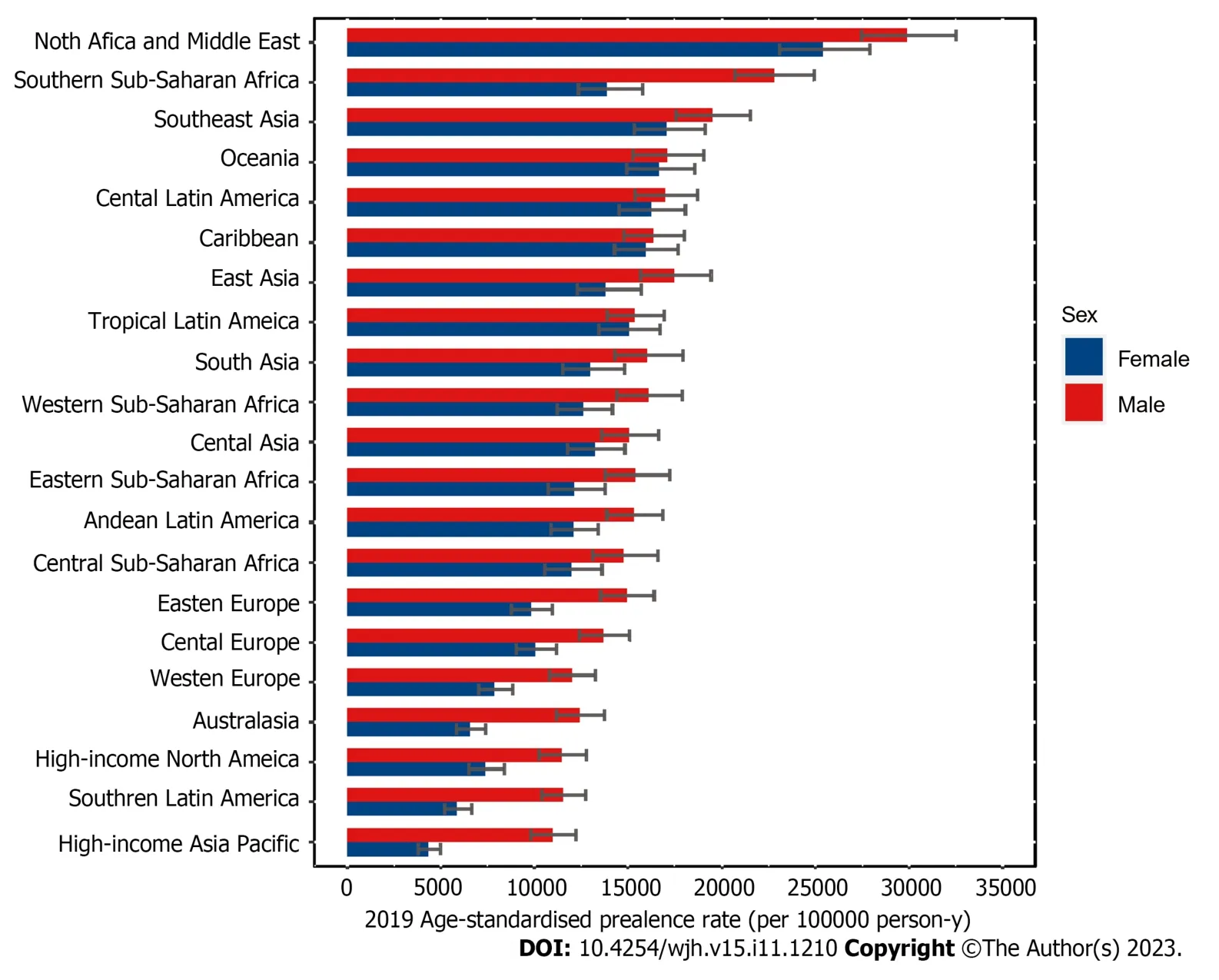
Figure 3 Age-standardized prevalence rate for cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease by region and sex,2019.
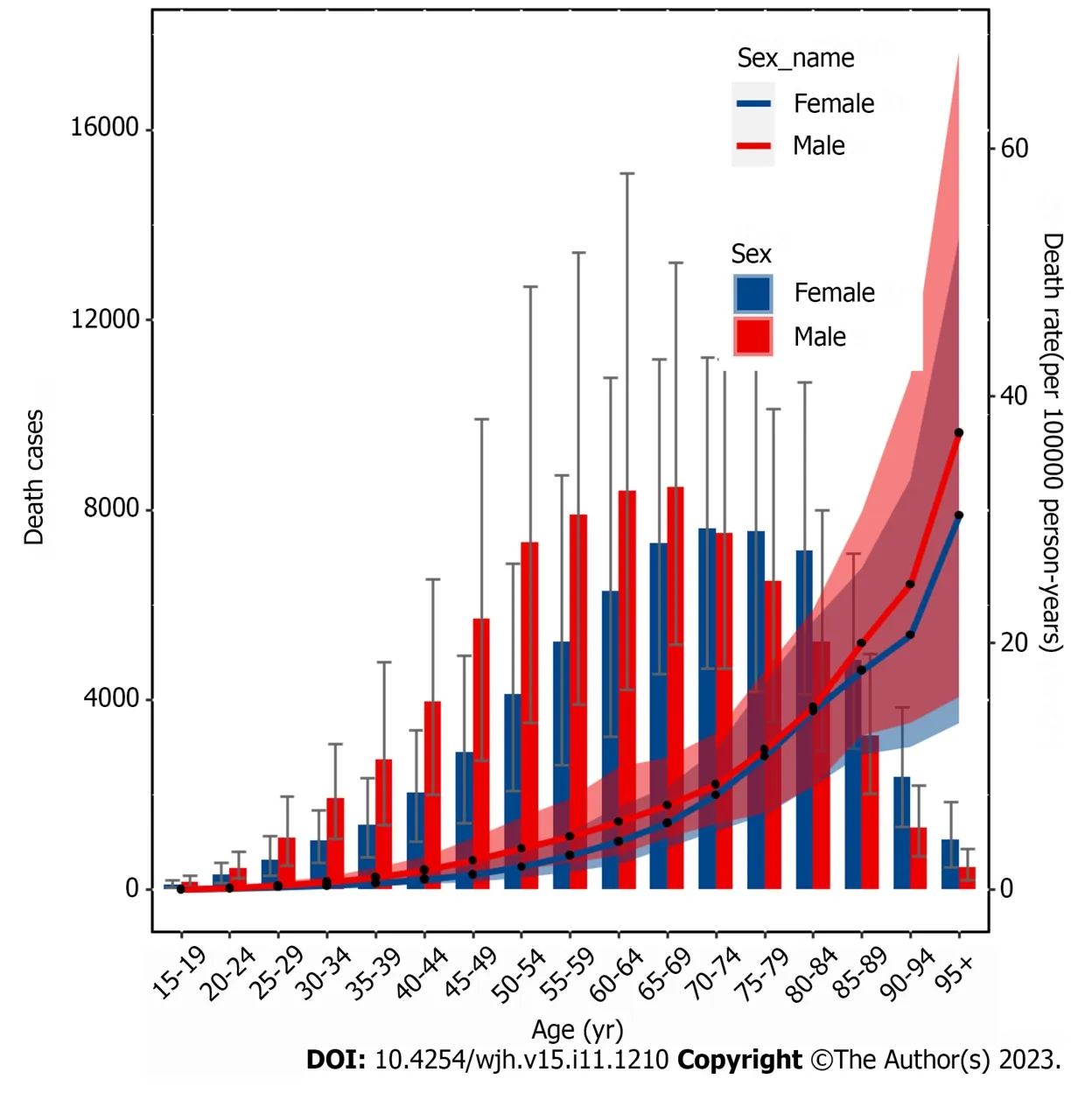
Figure 4 All-age numbers and rates of deaths for cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease in 2019 are illustrated by sex for females and males.
Among the 21 GBD regions,both the highest ASDR and ASDAR were observed in Central Latin America in 2019.Both the lowest ASDR and ASDAR were observed in high-income Asia Pacific in 2019 (Supplementary Tables 1 and 2,Supplementary Figures 5 and 6).The highest increases in the ASDR (EAPC=3.04;0.05-6.12) and ASDAR (EAPC=3.58;3.06-4.11) were found in Eastern Europe,followed by Central Asia and high-income North America.In contrast,highincome Asia Pacific exhibited the most pronounced decreases in the ASDR (EAPC=-3.18;-8.97-2.97) and ASDAR (EAPC=-3.36;-4.57 to -2.14) (Table 1).
The highest ASPR of COCLDs due to NAFLD was found in North Africa and the Middle East regions,followed by Southeast Asia and Southern Sub-Saharan Africa (Figure 3,Supplementary Table 3).The highest increase in the ASPR was observed in high-income North America,followed by Australasia and Southern Latin America.Central Sub-Saharan Africa showed the lowest increases from 1990 to 2019 (Table 1).
National levels
At the national level,the ASPR of COCLDs due to NAFLD ranged from 6680.34 to 34515.88 per 100000 population in 2019.In that year,Egypt [34515.89 (31796.95-37253.06) per 100000] had the highest ASPR in 2019,followed by Qatar and Kuwait.Conversely,Finland,Canada,and Greenland had the lowest ASPR in 2019.The most pronounced changes in prevalent cases from 1990 to 2019 were seen in Qatar and Georgia.The largest increase in ASPRs was observed in the Republic of Korea [EAPC=1.08;95% confidence interval (CI): 1.03-1.13] and Equatorial Guinea between 1990 and 2019.
Only Zimbabwe (EAPC=-0.06;95%CI: -0.10 to -0.03) showed a decreasing trend during this period (Supplementary Table 4,Figure 1C).
The highest ASDR of COCLDs due to NAFLD was observed in Egypt [14.02 (8.42-22.43)] in 2019,followed by Honduras and Guatemala.In contrast,Montenegro,Japan,and Singapore had the lowest ASDRs.Between 1990 and 2019,the United Arab Emirates [828.78% (368.37%-1461.06%)] showed the most significant increase in the number of deaths caused by COCLDs due to NAFLD,whereas Hungary showed a decrease of 39.94%.The largest increases in the ASDRs of COCLDs due to NAFLD were observed in Armenia (EAPC=4.21;95%CI: 0.98-7.54) and Kazakhstan (EAPC=4.11;95%CI: 1.33-6.97) from 1990 to 2019.In contrast,143 countries or territories experienced decreasing trends,with the Republic of Korea presenting the largest decrease in ASDR during this period (EAPC=-4.19;95%CI: -8.84 to -0.70) (Supplementary Table 5,Supplementary Figure 2).
The highest ASDAR of COCLDs due to NAFLD was observed in Guatemala [258.61 (170.42-329.98)] in 2019,followed by Honduras and Egypt.In contrast,Montenegro,Japan,and Singapore had the lowest ASDAR.Between 1990 and 2019,the United Arab Emirates [905.78% (402.13%-1627.41%)] showed the most significant increase in the number of DALYs from COCLDs due to NAFLD,whereas Hungary exhibited a decrease of 49.82% (-61.59% to -35.81%).The countries with the largest increases in ASDR during this period were Kazakhstan (EAPC=4.02;95%UI: 3.50-4.55) and Belarus.In contrast,the Republic of Korea experienced the largest decrease in ASDR,with the greatest reduction in ASDAR over the same period (Supplementary Table 6,Supplementary Figure 3).
Age and sex patterns
Globally,the prevalent number of COCLDs due to NAFLD exhibited an age-dependent pattern,reaching its peak at 45-49 years for males and 50-54 years for females.There was a declining trend in prevalence as age increased(Supplementary Figure 7).Similarly,the disease prevalence rate showed increasing and then decreasing trends with age in both sexes,with the highest prevalence rate observed in people aged 70-74 years,decreasing after this age group.
Globally,mortality rates increased with age and peaked at 65-69 years for males and 70-74 years for females before declining.The mortality rate steadily increased with age up to the 95+age group for both sexes in 2019 (Figure 4).In the same year,the 50-54 age group for males and the 60-64 age group for females had the highest number of DALY cases,which decreased as age increased.The rate of DALYs peaked in the 80-84 age group,decreased in the 85-94 age group,and subsequently increased in the 95+age group (Supplementary Figure 8).Among individuals under 70 years old,the numbers of prevalent cases,deaths,and DALYs lost was higher among males than females.However,among those aged 70 years and older,all three numbers were lower among males than among females (Figure 4,Supplementary Figures 7 and 8).
Burden of COCLDs due to NAFLD by SDI
From 1990 to 2019,there was generally a negative correlation between SDI and global and regional ASDARs of COCLDs due to NAFLD.Globally,the observed burden of COCLDs due to NAFLD was lower than expected.In most regions,higher SDI values were associated with decreased ASDAR,except in Central Asia,high-income North America,and Eastern Europe,which showed an increasing trend during the study period.At the regional level,the observed burden of ASDAR of COCLDs due to NAFLD in Central Latin America,Andean Latin America,Eastern Sub-Saharan Africa,Western Sub-Saharan Africa,Southeast Asia,and Western Europe was found to be higher than the expected level based on the SDI from 1990 to 2019 (Figure 5).The link between the SDI and ASDR of COCLDs due to NAFLD had a similar pattern from 1990 to 2019 (Supplementary Figure 9).The predicted relationship between SDI and ASPR of COCLDs due to NAFLD exhibited an initial increasing trend,followed by a decreasing trend at an SDI value of 0.58 (Supplementary Figure 10).
Figure 5 Age-standardized disability-adjusted life years rate of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease by sociodemographic index globally and in 21 regions,1990-2019. SDI: Sociodemographic index;DALYs: Disability-adjusted life years.
At the national level,the ASDAR of COCLDs due to NAFLD in 2019 generally displayed a negative correlation with SDI.In numerous countries/territories,including Egypt,Guatemala,Honduras,and Mexico,the ASDAR was higher than the expected level based on SDI in 2019;conversely,in countries such as the Maldives,Bangladesh,Papua New Guinea,and Mozambique,the burden was lower than expected (Figure 6).Negative correlations between the national-level ASDR and ASPR of COCLDs due to NAFLD and SDI in 2019 were also found (Supplementary Figures 11 and 12).
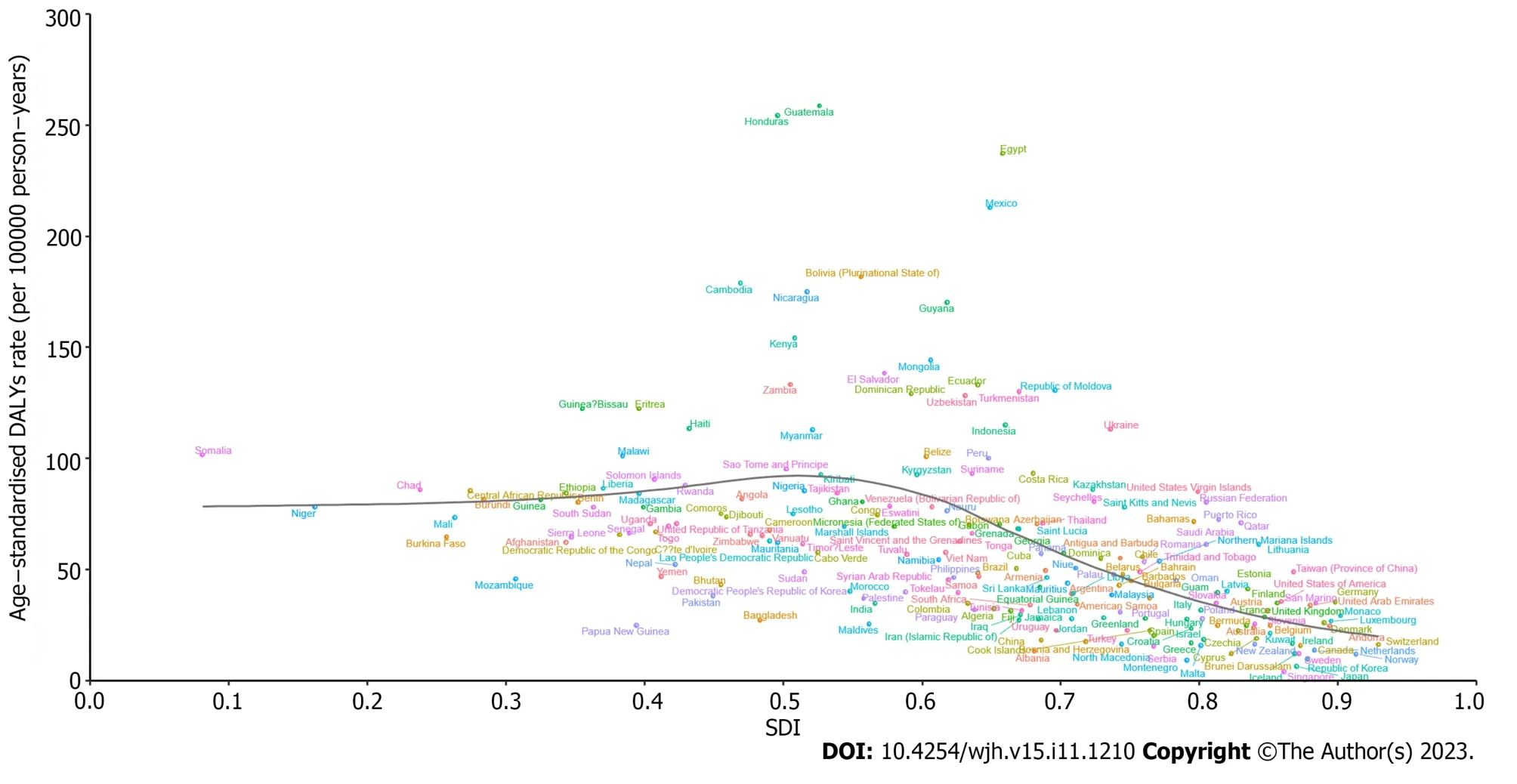
Figure 6 Age-standardized disability-adjusted life years rate of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease by sociodemographic index in 204 countries and territories,2019. DALYs: Disability-adjusted life years;SDI: Sociodemographic index.
DISCUSSION
This study comprehensively described the trends and patterns in prevalence,DALYs,and deaths caused by COCLDs due to NAFLD at the global,regional,and national levels over the past three decades.Globally,there were an estimated 123.56 million prevalent cases,0.13 million deaths,and 3.62 million DALYs lost in 2019.Our findings indicated a substantial increase in the number of all-age deaths,prevalent cases,and DALYs.The global prevalence and ASPR of COCLDs due to NAFLD both showed increasing trends from 1990 to 2019.Although the ASDR and ASDAR of COCLDs due to NAFLD decreased between 1990 and 2019,the total number of deaths and DALYs experienced an increasing trend,which can be partly explained by population growth,longer life expectancy,and higher prevalence in older age groups.COCLDs due to NAFLD are an increasing threat to our population and place a strain on valuable health resources.As there is currently no effective treatment for NAFLD,this trend is likely to continue,driven by its increasing prevalence.
To highlight the vital role of metabolic dysfunction in the pathogenesis of fatty liver disease,the Asian Pacific Association for the study of the Liver proposed that NAFLD be renamed metabolic-or metabolic dysfunction-associated fatty liver disease (MAFLD) in 2020[22,23].However,there exist slight discrepancies in the definitions of MAFLD and NAFLD among different populations.The key distinctions between NAFLD and MAFLD lie in the requirement for NAFLD to exclude alcohol consumption and other risk factors,such as chronic viral hepatitis,whereas the MAFLD diagnosis focuses on detecting fatty liver in conjunction with metabolic risk factors,without necessitating the exclusion of other liver disorders[24].In addition,GBD 2019 only estimated the burden of COCLDs due to NAFLD,and the MAFLD burden was not estimated.Therefore,in this study,we focused on the burden of COCLDs due to NAFLD.
NAFLD is closely associated with overweight and obesity,affecting an estimated 25% of the general adult population.Obesity significantly elevates the risk of NAFLD development.In a previous study,obesity was found in approximately 81% of patients with NASH and 50% of patients with NAFLD[25].Lifestyle modifications and bariatric surgery have significantly improved NAFLD activity scores[26,27].Earlier epidemiological investigations projected that the worldwide count of obese or overweight individuals surpassed 2.1 billion,constituting a pervasive global health concern[28].For 2019,we identified the prevalent count of COCLDs attributed to NAFLD as 1.2 billion individuals,which was slightly less than the number of obese individuals.
Interestingly,reports indicate that around 20% of Asian individuals diagnosed with NAFLD have body mass index and waist circumference measurements falling within the range designated as lean,despite the prevailing association of NAFLD with overweight or obesity[29].Notably,regions with higher incomes,such as the United States,France,and Japan,tend to exhibit an elevated prevalence of lean MAFLD[30].However,certain developing countries,such as India and Sri Lanka,have an even higher prevalence rate of lean MAFLD,which may be attributed to racial and dietary factors.United States-based studies also indicate that people with ancestry from Latin America have a higher prevalence rate of lean MAFLD,whereas African Americans have a lower prevalence rate.The suggested racial and ethnic variations are important risk factors for the prevalence of lean MAFLD[30,31].In addition,lean MAFLD patients have worse long-term outcomes than healthy people and have a similar prognosis to overweight or obese MAFLD patients.Therefore,more attention should be focused on normal-weight MAFLD patients,and a 3%-5% weight reduction and improvement in diet quality are strongly recommended to improve lean MAFLD[30].Beyond body weight,additional factors such as diabetes,ethnic disparities,and genetic variations could also contribute to the prevalence and outcomes of lean NAFLD[32].Given the ongoing global epidemic of obesity and diabetes,the burden of COCLDs attributed to NAFLD is expected to rise in the coming years.
According to previous research,the number of deaths due to cirrhosis caused by NAFLD/NASH was 102615 in 2012 and 118030 in 2017.The annual percent change in the ASDR of cirrhosis due to NAFLD/NASH from 2012 to 2019 was 0.29[33].In contrast,our study found that the EAPC of the ASDR of COCLDs due to NAFLD was -0.65 from 1990 to 2019,indicating a decreasing trend.This variation in findings can be ascribed to disparities in the time frames of participant enrolment: Our study encompassed data from 1990 to 2019,while the study by Paiket al[33] included data from 2012 to 2017.Notably,we also calculated the EAPC of the ASDR of COCLDs due to NAFLD from 2012 to 2019 and found a decreasing trend with a value of -0.05.This indicates that there may have been a decreasing trend from 2017 to 2019.
The global upsurge in type 2 diabetes and obesity has raised the prevalence of NAFLD in both developed and developing nations[4].Our study found that the highest ASPRs of COCLDs due to NAFLD were in some developing regions,such as North Africa,the Middle East regions,and Southeast Asia,and in specific countries such as Egypt,Qatar,and Kuwait.Previous research reported an NAFLD prevalence of 42.04% in South Asia and 31.79% in the Middle East,which is consistent with our finding that these regions had the highest prevalence rates[25,34].
According to previous research,approximately half of the global burden of liver complications associated with NAFLD is concentrated in the Middle East,North Africa,and Asia[35].The escalated prevalence in these geographical areas can be attributed to intricate interplays of lifestyle choices,economic conditions,and ethnic factors.The tandem epidemics of obesity and NAFLD are predominantly propelled by unhealthy dietary practices and sedentary habits characterized by consumption of calorie-dense foods and insufficient physical activity[34].Studies have indicated that Middle East and North African countries have a high prevalence of overweight and obesity,with more than 30% of females and more than 20% of males being obese in most countries in the region.This trend is attributed to unhealthy diets and the lowest levels of physical activity worldwide[36].Concurrently,the Middle East and North Africa register the highest prevalence rates of cirrhosis of the liver attributable to NAFLD.This underscores the critical need for effective interventions aimed at mitigating the escalating prevalence of obesity and diabetes to ameliorate the burden of COCLDs attributed to NAFLD[37].
According to our study,the prevalence,deaths,and DALYs lost due to COCLDs stemming from NAFLD were higher in males than in females across all age groups before the age of 65-69 years.Similarly,the rates of these occurrences were comparable when compared with their female counterparts across all age groups.This sex disparity is consistent with previous research demonstrating that from 1990 to 2017,the burden of cirrhosis in males was universally higher in males than in females[38].Hormonal factors could underlie this pattern,where estrogen,acting as an antioxidant,mitigates the activity of stellate cells and the advancement of liver fibrosis[39].After menopause,women lose the protective effect of estrogen[40],and physiological changes associated with hypoestrogenism,such as insulin resistance,dysglycemia,dyslipidemia,and visceral fat accumulation,may be associated with the higher prevalence of COCLDs due to NAFLD in postmenopausal women[41,42].This may partly elucidate the higher prevalence in males older than 70 years in our study.
We found that the number of prevalent cases,deaths,and DALYs lost due to COCLDs due to NAFLD was the highest among middle-aged groups (approximately 45-69 years).Within this range,the 75-79 age group presented the highest prevalence rate,while the 95+age group exhibited the highest mortality rate.The underlying reasons for these findings are multifactorial.One potential explanation involves the metabolic alterations that transpire in older age groups[43].Another possible reason is the natural history of liver cirrhosis,which is characterized by a compensated phase that lasts significantly longer than the rapidly progressive decompensated phase,with a median survival time of more than 12 years.A large proportion of patients with cirrhosis die after transitioning from the compensated phase to the decompensated phase[5].Given this context,the imperative need for accurate,noninvasive methodologies to enable early identification of COCLDs stemming from NAFLD becomes evident.
We found a negative correlation between the SDI and the ASDAR of COCLDs due to NAFLD in the 21 GBD regions from 1990 to 2019 and in 204 countries in 2019.Generally,regions with higher SDI had a lower burden of cirrhosis due to NAFLD,which may be attributed to accessible high-quality health care and enough safe spaces to exercise[44,45].
Conversely,low-SDI and low-middle-SDI regions tended to bear a higher burden.The Sub-Saharan African region showed a high ASDAR of COCLDs due to NAFLD in 2019.Some regions such as Western Sub-Saharan Africa,Southeast Asia,Central Latin America,Andean Latin America,and Eastern Sub-Saharan Africa,as well as some countries and territories,such as Egypt,Honduras,and Guatemala,had burdens higher than expected based on their SDIs,indicating that these regions and countries should receive more investment and public health programs.
The escalating prominence of COCLDs emanating from NAFLD has positioned it as a preeminent public health challenge.Notably,an absence of effective pharmaceutical interventions to fully eradicate NAFLD persists.Consequently,interventions targeting weight loss could be efficacious and cost-effective strategies to avert the progression of NAFLD to COCLDs.In addition,exercise interventions without significant weight loss have also had a beneficial effect on alleviating NAFLD[46].Thus,it is imperative to emphasize the critical role of weight management and exercise within public health programs.Furthermore,an enhancement of noninvasive diagnostic methods and the development of effective treatment strategies will be pivotal in alleviating the burden of COCLDs stemming from NAFLD.Importantly,public awareness regarding NAFLD and its associated complications remains inadequate.A concerted effort to raise population awareness about the implications of NAFLD is paramount.
In this study,we pioneered a comprehensive analysis of the relative burden of COCLDs attributed to NAFLD on global,regional,and national scales spanning the period from 1990 to 2019.Nevertheless,several limitations warrant consideration.First,the data from GBD 2019 have the general limitations of the GBD approach that have been described.The GBD estimates depended on robust statistical methods and trends from neighboring countries to overcome data scarcity and low data quality in some countries.Second,liver biopsy remains the gold-standard diagnostic test for patients with COCLDs due to NAFLD,but its poor acceptability during compensation and sampling variability may lead to misdiagnosis and underdiagnosis[47].A dearth of diagnostic techniques may cause an underestimation of COCLDs due to NAFLD,which may be more severe in regions with low SDIs.Third,patients admitted to hospitals mostly had decompensated cirrhosis.Therefore,the number of compensated cirrhosis cases may be underestimated.The underreporting of cirrhosis can bias the estimates.Fourth,GBD 2019 failed to adopt the new term MAFLD to replace NAFLD.NAFLD was defined only after the exclusion of other causes of hepatic steatosis,and there is an unclear differentiation between NAFLD and alcoholic liver disease owing to different adjustments for alcohol use.Finally,the exclusion of patients with cirrhosis with hepatocellular carcinoma from our study could result in an underestimation of the true mortality rate among individuals with liver cirrhosis due to NAFLD.
CONCLUSION
This study described the burden of COCLDs due to NAFLD in 204 countries and territories from 1990 to 2019 by age,sex,and SDI.COCLDs due to NAFLD are becoming a significant global public health concern.Over the past three decades,there has been a notable increase in the ASPR,while the ASDR and ASDAR have exhibited downward trends.Notably,substantial geographic disparities exist in the burden of COCLDs due to NAFLD,with the highest prevalence rates observed in North Africa and the Middle East.In 2019,males had a higher burden of prevalence,deaths,and DALYs lost than females before the 65-69 age group.Furthermore,there is a negative correlation between SDI values and ASDAR.We hope this study raises public awareness of COCLDs due to NAFLD and broadcasts the need for more effective prevention strategies to minimize the future health care burden.
ARTICLE HIGHLIGHTS
Research background
The incidence and prevalence of nonalcoholic fatty liver disease (NAFLD) have been rapidly increasing worldwide over the past few decades,leading to cirrhosis and other chronic liver diseases (COCLDs).Cirrhosis is the leading cause of liver-related morbidity and contributes to more than 1 million deaths annually worldwide.NAFLD has become the leading cause of COCLDs.
Research motivation
A previous study reported the burden of liver cirrhosis caused by nonalcoholic steatohepatitis.However,no studies have focused on the epidemiology of COCLDs due to NAFLD across the globe.
Research objectives
We conducted a comprehensive and comparable updated analysis of the global,regional,and national levels of prevalence,death,and disability-adjusted life-years (DALYs) of COCLDs due to NAFLD in regards to age-standardized rates and numbers from 1990 to 2019,stratified by sex,age,and sociodemographic index.
Research methods
Data on COCLDs due to NAFLD were collected from the Global Burden of Diseases,Injuries,and Risk Factors Study 2019.Numbers and age-standardized prevalence,death,and DALYs were estimated through a systematic analysis of modeled data from the Global Burden of Diseases,Injuries,and Risk Factors Study 2019.Estimated annual percentage change was used to determine the burden trend.
Research results
We found that the global age-standardized prevalence rate of COCLDs due to NAFLD was 15022.90 per 100000 population in 2019,with an estimated annual percentage change of 0.78.The age-standardized death rate and agestandardized DALYs rate per 100000 population were 1.66 and 43.69 in 2019,respectively.The highest prevalence rate was observed in North Africa and the Middle East.The numbers of prevalent cases,deaths,and DALYs cases of COCLDs due to NAFLD were higher in males than in females across all age groups before the age of 65-69 years.There was a negative correlation between sociodemographic index and age-standardized DALYs rate.
Research conclusions
COCLDs due to NAFLD have emerged as a large and growing public health burden worldwide.Globally,the ASPR has increased during the past three decades,whereas the ASDR and age-standardized DALY rate have decreased.There is geographical variation in the burden of COCLDs due to NAFLD.It is strongly recommended to improve the quality of COCLDs due to NAFLD health data across all countries and regions to facilitate better monitoring of the burden of COCLDs due to NAFLD.
Research perspectives
We believe that the findings of this study will provide insight into the global disease burden of COCLDs due to NAFLD and assist policymakers in formulating effective policies to mitigate modifiable risk factors.
ACKNOWLEDGEMENTS
We thank the work of the Institute for Health Metrics and Evaluation staff and its collaborators.
FOOTNOTES
Co-first authors:Zhi-Peng Liu,Guo-Qing Ouyang.
Co-corresponding authors:Song-Qing He,Guan-Dou Yuan.
Author contributions:Liu ZP,Ouyang GQ,He SQ,and Yuan GD conceived and designed the study;Liu ZP,Ouyang GQ,Huang GZ,Wei J,and Dai L were involved in collection and interpretation of the data;Liu ZP,Ouyang GQ,and Yuan GD edited the manuscript;Liu ZP,Ouyang GQ,and He SQ revised the manuscript;All authors were involved in reading and approving the final manuscript.We designated co-corresponding authors because our research was a collaborative team effort,and the designation of co-corresponding authors helped to assign responsibilities and tasks related to the paper.This helped improve the quality and reliability of the paper.Second,He SQ and Yuan GD made equally important contributions throughout the study.The selection of co-corresponding authors recognizes this equal contribution.In conclusion,we believe that the designation of He SQ and Yuan GD as co-corresponding authors is an appropriate choice for our manuscript because it accurately reflects the collaborative spirit and diversity of our team.Liu ZP and Ouyang GQ contributed equally as co-first authors to this work;He SQ and Yuan GD contributed equally as co-corresponding authors to this work.
Supported byNational Key research and Development Program,No.2022YFE0 131600;National Natural Science Foundation of China,No.82 160500;Special Project of Central Government Guiding Local Science and Technology Development,No.ZY20 198011;Guangxi Science and Technology Base and Talent Project,No.GuikeAA21 220002;Natural Science Foundation of Guangxi,No.2022GXNSFAA 035642;The Liuzhou Science and Technology Plan Project,No.2021CB0101.
Institutional review board statement:The study was reviewed and approved by the Institutional Review Board of The First Affiliated Hospital of Guangxi Medical University.
Clinical trial registration statement:This study was an analysis of the burden of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease.The data were extracted from the Global Burden of Diseases,Injuries,and Risk Factors database,and clinical trial registration statements were not necessary.
Informed consent statement:This study was an analysis of the burden of cirrhosis and other chronic liver diseases due to nonalcoholic fatty liver disease.The data were extracted from the Global Burden of Diseases,Injuries,and Risk Factors database,and ethics approval and consent to participate were not necessary.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
Data sharing statement:Data are available from http://ghdx.healthdata.org/gbd-results-tool and can be acquired from the corresponding author at dr_hesongqing@163.com.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Guo-Qing Ouyang 0000-0002-0130-7958;Song-Qing He 0000-0002-8966-2195;Guan-Dou Yuan 0000-0002-4758-1928.
S-Editor:Qu XL
L-Editor:Filipodia
P-Editor:Cai YX
 World Journal of Hepatology2023年11期
World Journal of Hepatology2023年11期
- World Journal of Hepatology的其它文章
- Budd-Chiari syndrome in children: Challenges and outcome
- Risk of hepatitis B reactivation in patients with myeloproliferative neoplasms treated with ruxolitinib
- Function of macrophage-derived exosomes in chronic liver disease:From pathogenesis to treatment
- Evaluation of a protocol for rifaximin discontinuation in critically ill patients with liver disease receiving broad-spectrum antibiotic therapy
- Metabolomics in chronic hepatitis C: Decoding fibrosis grading and underlying pathways
- Editorial: Metabolomics in chronic hepatitis C: Decoding fibrosis grading and underlying pathways
