Staphylococcus aureus bacteremia and infective endocarditis in a patient with epidermolytic hyperkeratosis: A case report
Yu Chen, Dian Chen, Hao Liu, Chen-Guang Zhang, Lin-Lin Song
Yu Chen, Chen-Guang Zhang, Lin-Lin Song, Department of Emergency, Beijing Tsinghua Changgung Hospital, Beijing 102218, China
Dian Chen, Department of Dermatology, Beijing Tsinghua Changgung Hospital, Beijing 102218, China
Hao Liu, Department of Pathology, Beijing Tsinghua Changgung Hospital, Beijing 102218,China
Abstract BACKGROUND Staphylococcus aureus bacteraemia (SAB) is among the leading causes of bacteraemia and infectious endocarditis. The frequency of infectious endocarditis (IE) among SAB patients ranges from 5% to 10%-12%. In adults, the characteristics of epidermolytic hyperkeratosis (EHK) include hyperkeratosis, erosions, and blisters. Patients with inflammatory skin diseases and some diseases involving the epidermis tend to exhibit a disturbed skin barrier and tend to have poor cellmediated immunity.CASE SUMMARY We describe a case of SAB and infective endocarditis in a 43-year-old male who presented with fever of unknown origin and skin diseases. After genetic tests, the skin disease was diagnosed as EHK.CONCLUSION A breached skin barrier secondary to EHK, coupled with inadequate sanitation, likely provided the opportunity for bacterial seeding, leading to IE and deepseated abscess or organ abscess. EHK may be associated with skin infection and multiple risk factors for extracutaneous infections. Patients with EHK should be treated early to minimize their consequences. If patients with EHK present with prolonged fever of unknown origin, IE and organ abscesses should be ruled out, including metastatic spreads.
Key Words: Staphylococcus aureus bacteremia; Infective endocarditis; Epidermolytic hyperkeratosis; Case report
INTRODUCTION
Epidermolytic hyperkeratosis (EHK), originally termed bullous congenital ichthyosiform erythroderma, is a rare autosomal dominant disorder caused by mutations in keratins 1 and 10. It has characteristics of erythema, blistering, erosions and skin denudation present at birth and develop marked hyperkeratosis in adults[1,2]. EHK is easy to distinguish from other congenital ichthyoses through its pathological features[2]. These manifestations are due to mutations in genes mostly involved in skin barrier formation. When the skin barrier function is significantly impaired, it can lead to hypernatremic dehydration, impaired thermoregulation, increased risk for eletrolyte imbalances and infection. A breached skin barrier secondary to EHK is likely to provide the opportunity for bacterial seeding and invasion, leading toStaphylococcus aureusbacteraemia (SAB) and infectious endocarditis, as in our case. We discuss a case of SAB and infective endocarditis in a 43-year-old man with EHK and no history of drug addiction.
CASE PRESENTATION
Chief complaints
A 43-year-old male presented with a 10-d history of pyrexia, fatigue, diarrhoea, and weight loss.
History of present illness
Upon presentation, he was pyrexial at 39°C, accompanied by fatigue, confusion, and diarrhoea.
History of past illness
He regarded his skin disease as psoriasis since childhood, with recurrently diffuse palmoplantar hyperkeratosis, erythema and hypernatremia on the flexor surfaces of both arms. He was not on regular medications and had never sought medical advice about his hyperkeratosis. He had never smoked, did not drink alcohol, and had no history of drug addiction. The patient had never received professional dermatological treatment.
Personal and family history
The patient had no significant prior family history.
Physical examination
The patient was pyrexial at 39°C with a blood pressure of 132/78 mmHg on admission. His hyperkeratosis affected his upper and lower limbs as diffuse palmoplantar hyperkeratosis, erythema, and scales on the flexor surfaces of both arms (Figure 1). He had a systolic murmur over the mitral area but did not exhibit the meningeal irritation sign or cardiopulmonary or abdominal issues.

Figure 1 Images of the skin lesions. Diffuse palmoplantar hyperkeratosis, erythema, and scales on the flexor surfaces of both arms and lower limbs. A: Palms;B: Opisthenar; C: Arms; D: Planta pedis; E: Dorsum of the foot.
Laboratory examinations
White cell counts and C-reactive protein levels were elevated to 17.07 × 109cells/L and above 250 mg/L, respectively. His procalcitonin levels were 3.38 ng/mL. His tests for human immunodeficiency virus (HIV) and syphilis antibodies were negative. His electrocardiogram showed sinus tachycardia. Blood cultures isolated methicillin-sensitiveStaphylococcus aureus(MSSA) 2 and 4 d after admission to the hospital. Transthoracic echocardiography indicated mitral valve disease with severe insufficiency.
Imaging examinations
Cranial computed tomography revealed multiple low-density shadows in the brain (Figure 2). The computed tomography (CT) results of the chest were normal. Abdominal enhanced CT showed multiple low-density shadows in the spleen, which were considered to be splenic abscesses with subcapsular effusion (Figure 2). Given the persistent fever, bacteraemia, abscesses, and mitral valve insufficiency, we conducted transoesophageal echocardiography (Figure 3), which revealed a wart in the mitral valve with prolapse along with severe insufficiency. He was diagnosed with definitive infective endocarditis, clinically suspected to be attributable to his skin lesions. He was urgently referred to a dermatologist, who advised treatment with tretinoin, urea cream for external use, skin biopsy (Figure 4), and genetic tests. Later, a pathological examination was conducted on his skin, which showed epidermal hyperkeratosis, acantholysis, and lymphocytes infiltrating the superficial dermis around the blood vessels and adjuncts. Genetic tests revealed mutations in the keratin 1 (KRT1) gene (Figure 4).
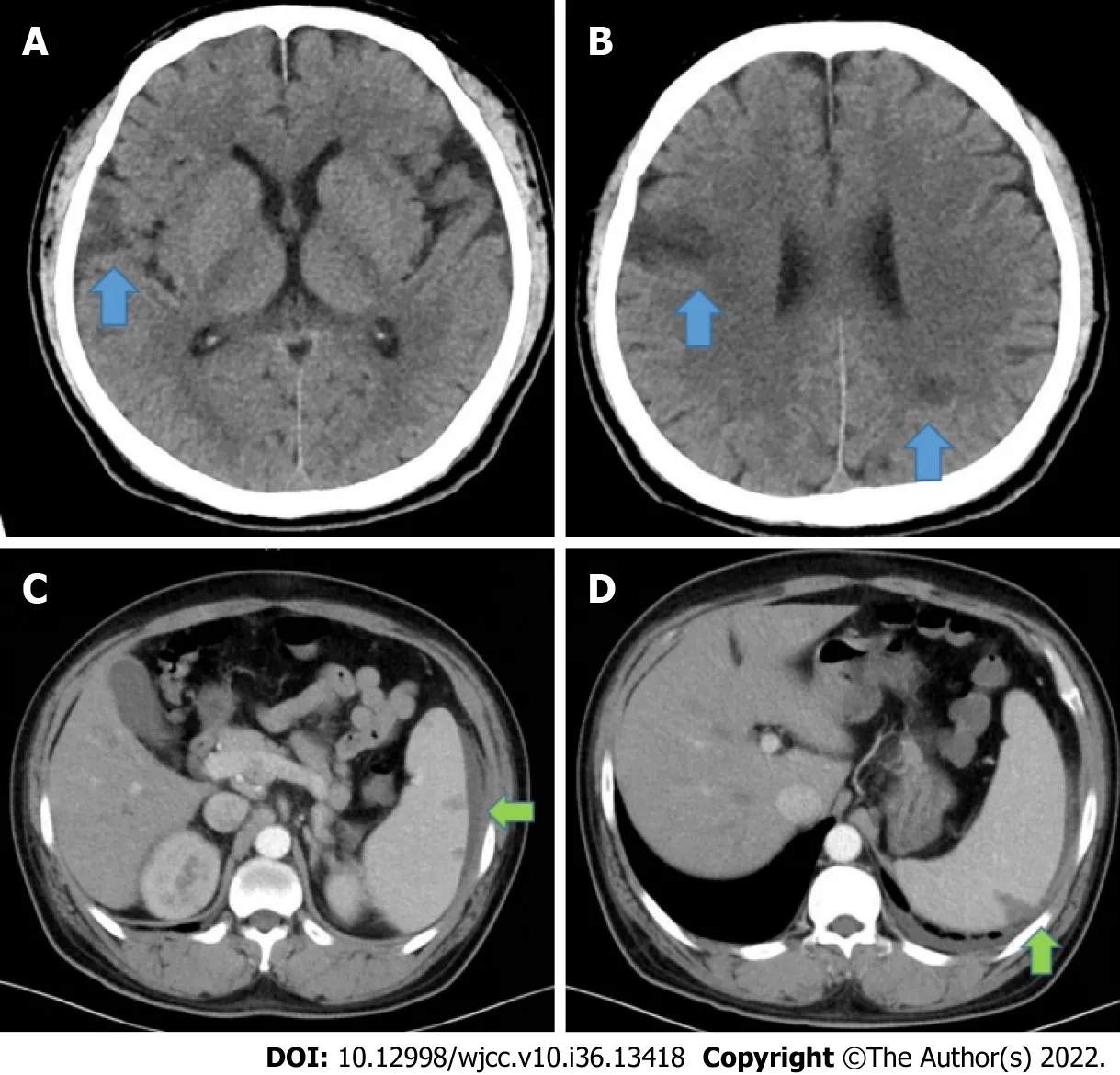
Figure 2 Computed tomography. A and B: Cranial computed tomography showing multiple low-density shadows (blue arrow, A and B) in the brain; C and D:Abdominal enhanced CT scan showing multiple low-density shadows (green arrow, C and D) in the spleen, considered a splenic abscess with subcapsular effusion.

Figure 3 Transesophageal echocardiography. A and B: The anterior leaflet of the mitral valve was detected with a wart (white arrow) of a cord-like medium echoic substance about 10mm and the posterior leaflet was detected with the wart (white arrow) of a medium echoic substance about 7 mm × 7 mm; C and D: There was severe mitral regurgitation and the regurgitation bundle was distributed along the posterior leaflet of the mitral valve. There was mild tricuspid valve and the aortic valve regurgitation.
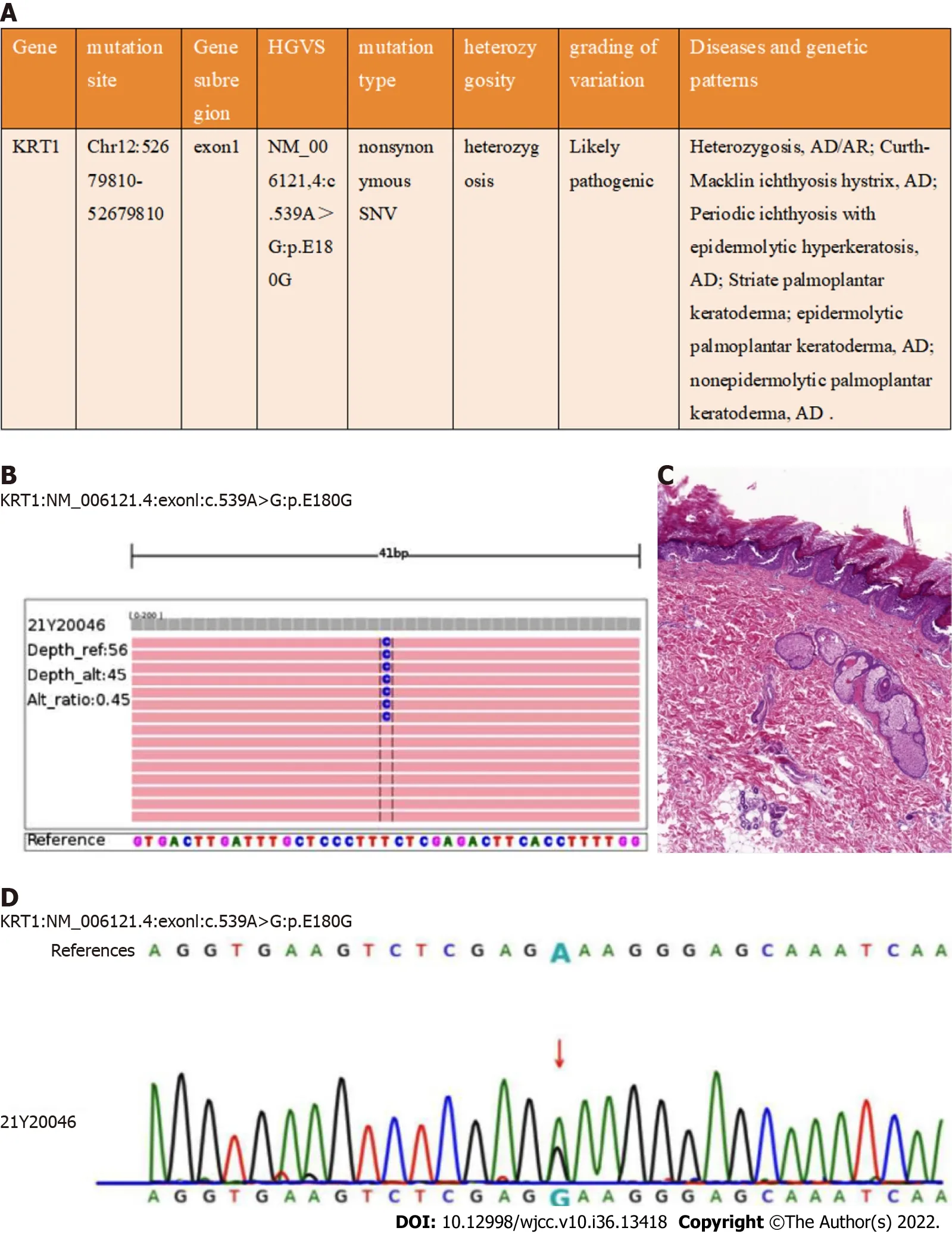
Figure 4 Histopathological, and genetic features of the patient. A and B: The c.539A>G mutation was detected in KRT1; C: The pathological examination indicated epidermal hyperkeratosis, acantholysis and lymphocytes infiltrating the superficial dermis around blood vessels and adjuncts (H&E stain, original magnification 100×); D: c.539A>G detection using Next Generation Sequencing and Sanger sequencing.
FINAL DIAGNOSIS
The final diagnosis of the presented case was EHK combined with infectious endocarditis (IE).
TREATMENT
He was started on intravenous 0.5 g levofloxacin once a day (QD). Four days later, levofloxacin was escalated to vancomycin 500 mg Q12 h due to a positive blood culture for Gram-positive coccal bacteraemia and persistent fever. When infective endocarditis and brain abscesses are diagnosed, the selection of antibiotics depends on drug sensitivity experiments; based on the results, his treatment was changed to 2 g ceftriaxone QD.
OUTCOME AND FOLLOW-UP
Cardiac surgery was planned for approximately 6-8 wk after completion of the course of antibiotics. Because of the use of antibiotics, his white cell counts and C-reactive protein levels remained within the normal range. Subsequent echocardiograms still showed a wart in the mitral valve with prolapse and severe insufficiency, but the valve excrescences appeared to be getting smaller. CT of the chest was repeated, which revealed a small pleural effusion. Cranial CT was also repeated, which indicated shrinking lesions. Blood cultures were repeated and were negative, and he remained apyrexial. Because of his medical insurance policy, the patient decided to return to his local hospital for further treatment.
DISCUSSION
The clinical manifestations, histopathological findings, and mutations in the KRT1 gene observed in this patient were consistent with the diagnostic criteria of EHK[3,4], a rare genodermatosis with autosomaldominant inheritance[5]. EHK is associated with erythema, blistering, erosions and skin denudation present at birth, and develop marked hyperkeratosis in adult. The KRT1 mutation c.539A>G: p. E180G was found; this has been reported previously[6].
Patients with skin diseases often exhibit a disturbed skin barrier and tend to have poor cell-mediated immunity, such as atopic dermatitis, irritant contact dermatitis, ichthyosis, rosacea, and acne[7,8]. Patients with EHK, especially with subtypes of ichthyosis, are prone to repeated episodes of skin infections, including bacterial infection and fungal infection, but the mechanism is still elusive[4,9]. Several factors have been proposed, including disruption of skin barrier function, hyperkeratotic plaques and defective cell-mediated immunity[10-12].Staphylococcus aureusis a leading cause of human bacterial infection, and the most common site ofStaphylococcus aureusinfection is the skin[13]. Skin and soft tissue infections with Staphylococcus remain a dominant cause of bacteraemia and IE[14,15].
The definition of SAB is as presence of ≥ 1 positive blood cultures forStaphylococcus aureus[16]. The most frequent site is the anterior nares, but the skin, axilla, oropharynx, perineum, and vagina may also be colonized. These colonized sites may serve as reservoirs for future infections. Colonization is relatively higher among patients with insulin-dependent diabetes, skin damage, HIV infection, and in patients undergoing maintenance haemodialysis[16]. SAB can lead to seeding and invasion of virtually any body site and associated complications[17]. The case fatality rates for SAB have only slightly improved in recent decades[18]. Patients with SAB can develop all kinds of complications, such as IE, epidural abscess, vertebral osteomyelitis, brain abscess, and discitis, which may be difficult to identify and can lead to high rates of disability and mortality[17,19].
SAB is a leading cause of bacteraemia and infective endocarditis. Only a minority of bacteraemic patients will show involvement of the heart valves. The frequency of endocarditis among SAB patients ranges from 5% to 10%-12%[20]. IE is a severe complication in patients with nosocomial SAB. It has a low incidence but high mortality. Therefore, prevention and early detection of IE are important. The incidence is highest in those with a previous history of IE or who have prosthetic, repaired valves, intravenous drug use or rheumatic heart disease[21,22]. Our patient had no history of these risk factors except EHK.
CONCLUSION
A case of atopic dermatitis, IE and multiple cerebral infarctions has been reported[23], but there are no previous reports of EHK and IE, such as in our case. Some factors have been speculated to increase the risk of infection, such as including disruption of skin barrier integrity, defective cell-mediated immunity, and delayed keratin scaling. In our case, a breached skin barrier secondary to EHK, coupled with inadequate skin sanitation, likely provided the opportunity for bacterial seeding by MSSA, triggering IE and abscesses. EHK may be associated with skin infection and multiple risk factors for extracutaneous infections. Patients with EHK should be treated early to minimize the consequences. If patients with EHK present with prolonged fever, IE and organ abscesses should be suspected or checked, including metastatic spreads. In conclusion, we highlight that in the absence of thorough treatment, clinicians should recognize that patients with EHK are susceptible to bacterial infections owing to disruption of the skin barrier.
ACKNOWLEDGEMENTS
We would like to thank the patient and his family. We extend our thanks to the dermatology, echocardiography, radiology, and pathology departments of the Beijing Tsinghua Changgung Hospital for facilitating the acquisition of the relevant materials.
FOOTNOTES
Author contributions:Chen Y and Song LL analyzed the data and wrote the manuscript; Liu H and Chen D contributed new pathological datum and analytic tools; Zhang CG designed the research study; All authors have read and approve the final manuscript.
Informed consent statement:All study participants provided informed written consent prior to study enrollment.
Conflict-of-interest statement:We declare that we have no financial and personal relationships with other people or organizations that can inappropriately influence our work, there is no professional or other personal interest of any nature or kind in any product, service and/or company that could be construed as influencing the position presented in, or the review of, the manuscript entitled.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Lin-Lin Song 0000-0001-6398-6725.
S-Editor:Liu JH
L-Editor:A
P-Editor:Liu JH
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Liver injury in COVID-19: Holds ferritinophagy-mediated ferroptosis accountable
- Amebic liver abscess by Entamoeba histolytica
- Living with liver disease in the era of COVID-19-the impact of the epidemic and the threat to high-risk populations
- Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis
- Probiotics for preventing gestational diabetes in overweight or obese pregnant women: A review
- Effectiveness of microwave endometrial ablation combined with hysteroscopic transcervical resection in treating submucous uterine myomas
