Sexual Behavior and Awareness of Sexually Transmitted Diseases Among Street-Based Female Sex Workers in the Florence Area, Central Italy
Barbara Giomi, Caterina Silvestri, Stefano Bravi, Cristina Stasi,3,*, Lisa Bertini, Leslie Mechi,Serena Mordini, Nicoletta Zocco, Fabio Voller, Francesco Cipriani
1 Unit for STD and AIDS, Department of Dermatology, University of Florence, Florence 50134, Italy; 2 Observatory of Epidemiology,Regional Health Agency of Tuscany, Florence 50141, Italy; 3 Interdepartmental Hepatology Center MASVE, Department of Experimental and Clinical Medicine, University of Florence, Florence 50134, Italy; 4 CAT Social Cooperative Road Unit SATIS Regional Project, Florence 50134, Italy; 5 Department of Prevention, Central Tuscany Local Unit, Florence 50135, Italy.
Abstract Objective: Street-based female sex workers are more likely to practice unprotected sex with multiple partners increases their risk of infection with sexually transmitted diseases. This study was performed to evaluate the understanding of and risk factors for sexually transmitted diseases among street-based female sex workers.Methods: A survey consisted of a sociodemographic section and a health section was conducted from June to August in two consecutive years (2012-2013) using an anonymous questionnaire compiled by street-based female sex workers in the area of Florence (Central Italy). A descriptive analysis of sociodemographic, epidemiological, and anamnestic variables was performed using common methods for proportions; associations between variables were assessed using univariate and bivariate logistic regression.Results: Totally 122 street-based female sex workers (mean age, 24.1 years; age range, 17–45 years) were enrolled, and were from Europe (63.1%) (mainly from Romania [48.4%] and Albania [13.1%]), Africa (31.2%)(specifically Nigeria), and South America (5.7%). Of the 122 street-based female sex workers, 63% were married/engaged and 37% were single. More than half had been living in Italy and Florence for more than 1 year; 72.8%stated that they possessed a residence permit and the others were illegal migrants. Eighteen (15%) street-based female sex workers also worked in the industry in neighboring European countries. Their level of education was generally high: 58.1% had completed secondary school (lower secondary school and upper secondary school). A total of 81.4% stated that they perceived an actual fear of contracting human immunodeficiency virus; in fact, 43.3%had never been tested for any sexually transmitted diseases except for human immunodeficiency virus.Conclusion: Despite the long-time involvement of street-based female sex workers in the commercial sex industry, the large numbers of clients and a strong perception of concerns about sexually transmitted diseases. This study confirms a low rate of condom use and blood screening, and corresponding science education and health screening efforts need to be strengthened in this high risk population.
Keywords: female sex street workers, foreigners, sexually transmitted diseases
Introduction
Sexually transmitted diseases (STDs) are dynamically distributed throughout populations because the factors contributing to the spread of pathogens change over time in parallel with the changes in sexual behavior. The most common STDs are chlamydia, herpes simplex, human papillomavirus, gonorrhea, hepatitis B virus, syphilis,trichomoniasis, and human immunodeficiency virus(HIV).1
Female sex workers (FSWs) are perceived as one of the “core groups” at risk of STDs, with multiple partners and low socioeconomic and cultural backgrounds strongly contributing to their vulnerability. Commercial sex workers may infect and become infected by their clients (considered a “bridging group” of men who use condoms inconsistently and do not practise safe sex with their spouses), and FSWs may subsequently transmit the infection to other partners in the general population.2
In Italy, there is no standardized system for surveying sexual behaviors that cause STDs and their prevalence in core groups such as immigrants or sex workers.Therefore, these high-risk populations may never be tested for STDs. In particular, the health of sex workers is often uncontrolled and strongly influenced by the degree of promiscuity and amount of sexual intercourse.Most street-based sex workers are immigrants, many of them illegal immigrants or victims of trade, who live in marginalized societies and have reduced access to health and social support services. Moreover, they are subject to greater requests for unprotected sex, which increases individual and public health risks. Therefore, understanding the behavior and social patterns of sex workers could prove to be of primary importance in the targeting and expansion of preventive measures against STDs.
Based on these premises, the Tuscany Regional Health Agency in collaboration with the CAT Social Cooperative,a local association of the Florence metropolitan area that provides support to disadvantaged groups, performed this study to examine the risk factors for STDs among street-based FSWs.
Materials and methods
Data collection
Given that recruiting in facilities or institutions is prone to bias, this study adopted instead a powerful sampling technique for sex workers working at set times in certain places, such as specific city streets.3Although these places(eg, streets) are not specifically designated for sex work per se, they can easily be identified as places known for sex work at certain times of day, such as the main streets in Florence. A well-known methodology for research on sexual behavior is the Priorities for Local AIDS Control Efforts methodology, which enables HIV/sexually transmitted infection (STI) interventions to be tailored to the specific location where such “high-risk” events are most common,thereby reducing the stigma that can arise from defining,identifying, and subsequently targeting high-risk individuals.3In the present study, all mapped locations for FSWs were reached by staff on a minibus during peak hours. All FSWs were individually approached on site and invited to participate in the study and interview on site. Women who declined an on-site interview the same night were excluded from the study. The data of this study were used for social interventions, but we believe that the published data could also be useful for implementing public health interventions currently lacking in the region. The nature of the study was explained to the participants, who provided written informed consent before enrolment, and the study was performed in accordance with the Declaration of Helsinki(revised in Edinburgh, 2000). According to the Italian legislation on data confidentiality, the dataset used is not openly available (Decree No. 196/2003). No identifiable human data were used for this study.
This survey was conducted from June to August in two consecutive years (2012-2013) using an anonymous questionnaire (Supplemental Table 1, http://links.lww.com/JD9/A33) compiled by FSWs practising their profession in the area of Florence (Central Italy). The reliability of the questionnaire was evaluated by an evidence-based approach for clinical practice.4The study was conducted in the FSWs’ main working zone in Florence. The FSWs were approached on the street by a group of volunteers(mainly welfare workers, members of the CAT cooperative), and they were issued the questionnaire in their native language.
The questionnaire consisted of two sections: a sociodemographic section and a health section. The sociodemographic section included questions regarding general information such as age, sex, nationality, years of study,and country of origin. The health section contained questions regarding sexual behavior, condom use, and current knowledge about HIV and other STDs among FSWs.
Statistical analysis
All results are expressed as mean and percentage. The chisquare statistic was used to test the relationships between categorical variables. A descriptive analysis of sociodemographic, epidemiological, and anamnestic variables was performed using common methods for proportions; associations between variables were assessed using univariate and bivariate logistic regression. The confidence intervals(CIs) were computed at 95%. Relative risk was used to measure the risk of contracting an infection. Statistical analyses were performed using STATA software 12.0 for personal computers (StataCorp, College Station, TX,USA).
Results
Sociodemographic section
A total of 122 FSWs were enrolled (mean age, 24.1 years; age range, 17-45 years). Their level of education was generally high; 58.1% had completed secondary school. Approximately 80% of the enrolled FSWs stated that they lived in an apartment with flatmates. Only a minority lived in a hotel, and most of these women had moved to Florence less than 1 year. Concerning their marital status, 77 (63%) FSWs were married/engaged and 45(37%) were single (Table 1).
Our study population mainly comprised women who had come from Europe (63.1%) (mostly Romania), but some women were from South America (5.7%) and Africa (31.1%) (specifically Nigeria in Sub-Saharan Africa). They had grown up mainly in urban areas, and more than half had been living in Italy and Florence for more than 1 year. Eighty-three (72.8%) FSWs stated that they held a residency permit, whereas the others were illegal migrants. Nigerian women were significantly less likely to have regular identity documents than women from other geographical areas (P< 0.0001). A total of 15% of FSWs had worked in their current activity in neighboring European countries before moving to Italy.However, more than half of the interviewed women had been involved in sex work for more than 1 year(Table 2).
Health section
The reported age at first sexual intercourse was <16 years for 39.3% of FSWs and >16 years for 60.7% (Table 2).In particular, age at first sexual intercourse was significantly associated with ethnicity; Albanian women were most likely to have their first sexual experience at a younger age (odds ratio, 0.21; 95% CI, 0.003–0.162;P< 0.001) and Nigerian women tended to be older(odds ratio, 14.82; 95% CI, 3.188–68.918;P= 0.001).Moreover, among FSWs with lower levels of education,the probability of having sexual intercourse before 16 years of age increased by 1.5 times (odds ratio, 1.5; 95%CI, 1.096–2.054;P= 0.011).

Table 1 Sociodemographic characteristics of interviewed female sex workers.
FSWs reported an average of 22 different sexual partners per week (range, 2–90) and stated that 80% of clients requested unprotected oral and vaginal sex. This request was associated with the proposal of a larger amount of money in 96.6% of cases. The questionnaire results did not show consistent use of condoms and consistent use was not significantly related to the women’s ethnicity,age or even education. Only 28% of FSWs reported regular condom use for vaginal sex, whereas 72% of FSWs admitted that they sometimes agreed to unprotected sexual intercourse, either with boyfriends/husbands (56%)or “well-known” or “trusted” clients (8%) or for money(8%; Table 2). Condom use was significantly lower with non-paying partners: 63.2% of enrolled FSWs never used condoms with their spouses, just 12.6% consistently used condoms, and 24% “seldom” or “often” used condoms(Table 2). When data about condom use were crossed, we found that among those women who always used condoms with clients, 70% admitted that they did not use condoms with boyfriends/husbands.
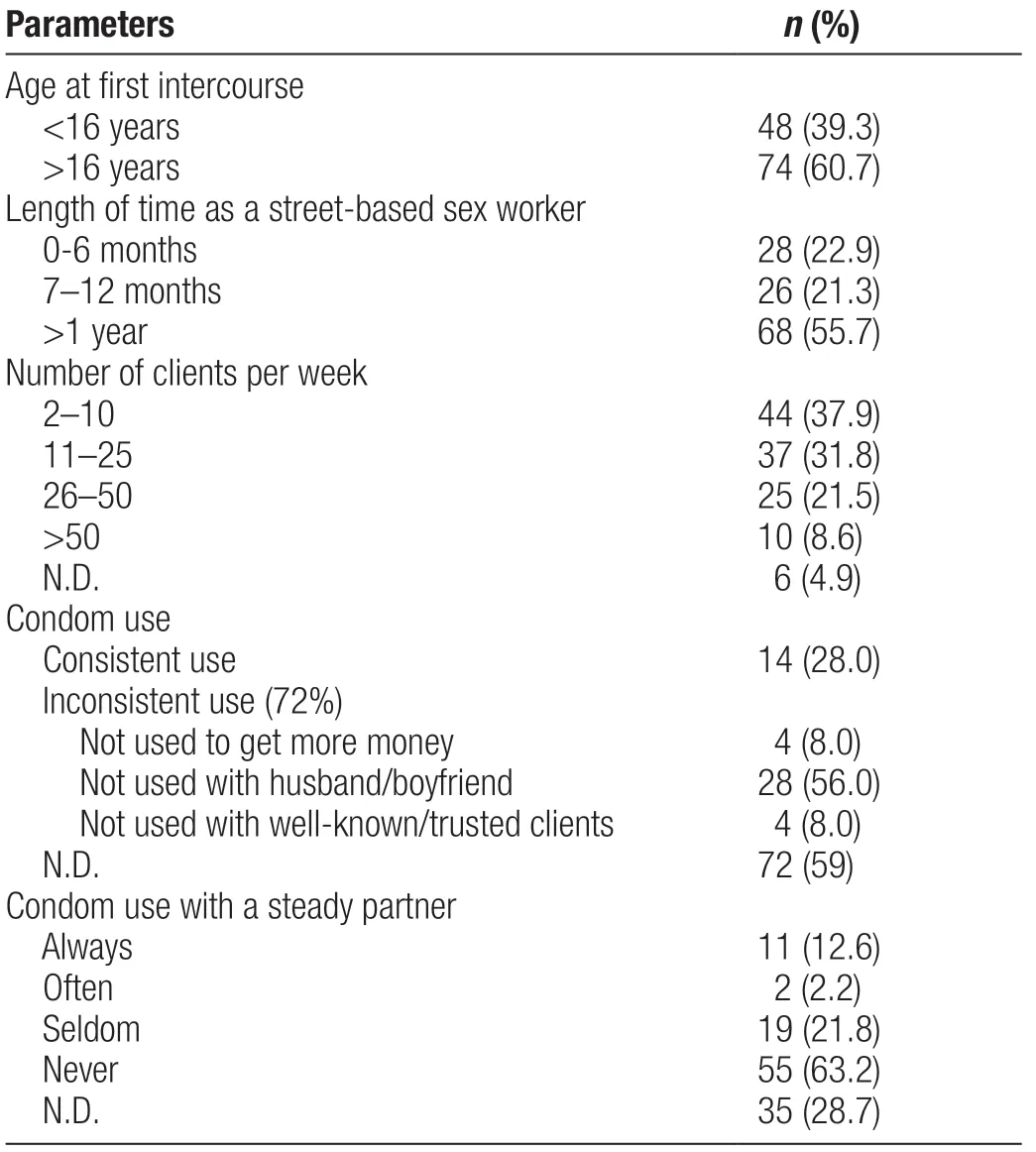
Table 2 Sexual behavior of interviewed female sex workers.
The majority of the women (81.4%) stated that they perceived an actual fear of contracting HIV (Table 3).Ethnicity, age, number of clients per week, education, and a longer period working in the sex industry did not seem to influence the FSWs’ understanding and perception of the risk of HIV. A total of 39% of FSWs in this survey had never been tested for HIV, and 30% had undergone HIV screening more than 12 months (Table 3). The main reasons for the decision not to get tested were lack of time(40.5%), lack of information on the clinics that perform free blood tests (27.0%), coercion by pimps (10.8%),and shame (5.4%) or fear (2.7%). A total of 18.6% of FSWs did not feel that they were at risk of contracting HIV despite the fact that more than half of this group did not consistently use condoms with clients or steady partners. In contrast, 64.2% of FSWs who declared that they always used condoms still felt that they were at risk of HIV.
Finally, the questionnaire included several questions about STDs. These items indicated that 43.3% of FSWs had never been tested for other STDs, although half of FSWs reported vaginal discharge, itching, pelvic pain, or one or more symptoms of STDs (genital vesicles, ulcers, nodules,or similar lesions) in the previous 6 months (Table 3).
Discussion
Despite differences among regions, studies worldwide have demonstrated a significantly higher prevalence ofSTD-related morbidity among FSWs than among the general female population.5-6In Italy, where prostitution itself is legal but organized prostitution is illegal, only a few fragmentary papers have focused on the prevalence of HIV and other STDs in sex workers.7-10These reports provide conflicting results, reflecting differences in the composition and number of surveys, country of origin,and methods. However, they unanimously recognize that multiple partners, inconsistent condom use, migration,and social and economic factors expose FSWs and their clients to significant risk in terms of individual and public health. Given the risk of inconsistent results caused by lack of understanding or knowledge gaps among participants, we analyzed their level of education and we found that 72% of the FSWs had completed at least 6 to 8 years of schooling. Only two previously published Italian papers included a questionnaire covering knowledge of STDs and condom use among FSWs. The first study was conducted by Fornasaet al.11in 2005 and involved a survey of 98 FSWs in Padua, North Italy. The second was conducted by Traniet al.12in 2006 among 241 FSWs in the Milan area. The main limitation of these two studies is the small number of enrolled women, who were stratified by their different ethnicities. Moreover, FSWs may not wish to give accurate descriptions of their lives, work,and sexual behavior for reasons associated with pride,fear or shame.

Table 3 Questions concerning awareness and fear of contracting sexually transmitted infections among female sex workers.
Although a large majority of respondents did not reply to questions regarding condom use in our study,data from other studies could be compared with our results. First, the percentage of FSWs in Florence declaring that they “always use condoms (28%) was lower than that reported in FSWs in Padua (61%) and in Milan (almost 100%).” As expected, in both previous studies, condom use dramatically decreased when considering non-paying partners, including boyfriends and pimps. Other studies have shown that FSWs with higher levels of education are more aware of their risk of contracting STDs and are more likely to use condoms.13-14According to these studies, our results showed moderate (24.6%) to strong (56.8%) risk perceptions for HIV and STDs among FSWs.
Although this corroborates our results, it most importantly indicates an alternative possibility of the spread of STDs outside the sex industry if the FSWs’ steady partners have sexual intercourse with other people. We can assume that coercion and fear play a more pivotal role than lack of awareness in scarce condom use with pimps. Zermianiet al.15assessed the prevalence of STDs and hepatitis C in a population of immigrant FSWs. The tests were performed at an outpatient clinic in Verona (North Italy).In screenings performed from 1999 to 2007, 345 FSWs were tested for STDs and 4.6% of these were positive for HIV, 2.0% for syphilis, 0.9% for hepatitis C virus, 3.5%for hepatitis B surface antigen, and 40.6% for hepatitis B core antibody.
Lack of condom use was also related to pressure by clients in return for money. This fact sheds further light on the poor economic situations of FSWs and the barriers they face in negotiating condom use, indicating the need for interventions targeting clients rather than FSWs alone in order to change behaviors that may not be under the FSWs’ control.
A cross-sectional anonymous telephone survey was recently carried out at the AIDS and Sexually Transmitted Infections Helpline run by the Italian National Institute of Health. The questionnaire was voluntarily administered by helpline users to a sample of 119 subjects aged 19 to 59 years. Vaginal intercourse with FSWs was most frequently reported, followed by passive oral sex, active oral sex, and active anal intercourse. Cumulatively, 86.6%and 84.6% of vaginal and anal intercourse, respectively,was performed with protection by a condom.16
In our study, the FSWs seemed to be conscious of the risks associated with their profession. In fact, as in the studies by Fornasaet al.11and Traniet al.,12the FSWs were aware of HIV and other STDs and experienced strong fear about contracting them. In our population,fear was more marked in older FSWs, those with a higher number of clients per week, and those of Nigerian ethnicity. However, despite a relatively high level of education among the interviewed women, which could be assumed to be correlated with greater understanding of the transmission of STDs, only few FSWs had undergone screening blood tests. Similarly, the proportion of FSWs who had experienced symptoms of STDs but had never received a diagnosis or undergone treatment was consistent with although slightly lower than previous reports.17The inclusion of questions about STD tests and treatment among FSWs is a novelty of our study, but the FSWs’ answers highlight a very alarming scenario: only a minority of FSWs had been screened for HIV in the previous 3 months, and the main reason was “lack of time and opportunity.” Again, we can suppose that FSWs live in forced conditions and very marginalized societies and have very limited access to health services (in the Florence area, there are at least five hospitals and several welfare clinics where FSWs can get free blood tests). The limitations of this study include the lack of consideration of the behavioral effects of drug use or withdrawal symptoms that can reduce the ability to negotiate condom use and other issues.
Only a few studies conducted in Italy to date have adequately studied the situation of sex workers, their habits regarding STD prevention and their confidence in preventive interventions. Therefore, we urge public health authorities to intensify interventions aimed at increasing sex workers’ willingness to adopt measures of STD prevention. For this population to access STD health services and avoid coercion from pimps, more regional outreach services should be established offering education on the prevention of STDs and HIV; condoms should be distributed and their use promoted; and FSWs should be recruited for STD screening. Most FSWs need access to services where condoms and information on STDs are provided free of charge; this could greatly affect the spread of STIs. Mobile units can provide both information and screening for most STDs. FSWs should be encouraged to visit an STI screening clinic and should be educated on STI prevention, diagnosis, and treatment,how to negotiate the use of condoms and the possibility of accessing legal aid in the event of suffering violence and assaults.18
The main limitation of this study is its small sample.The FSWs were approached individually and invited to participate in the interview on site; therefore, women who declined an on-site interview were excluded from the study. In addition, a large majority of FSWs did not reply to the interview items regarding condom use. The results showed that the main FSW populations reached in our study were Romanian, Nigerian, and Albanian, with first sexual intercourse at <16 years particularly prevalent among Albanian women. Most FSWs were married or engaged, had a high level of education and had been working in the sex industry for a relatively long period of time. Despite the high number of clients and strongly perceived concern about STDs, the rates of condom use and STD blood testing were low. The main reasons for this were coercion by pimps or lack of information about available health services. Notably, when compared with similar previous studies performed about 10 years ago,our data show that the situation for sex workers has not evolved significantly and that effective intervention strategies are still lacking.
- 國際皮膚性病學雜志的其它文章
- Efficacy and Safety of lxekizumab in Chinese Patients With Moderate-to-Severe Plaque Psoriasis: 60-Week Results From a Phase 3 Study
- Characterization of Generalized Pustular Psoriasis in Northwest China: A Single-Center Retrospective Study
- Understanding the Pathogenesis of Generalized Pustular Psoriasis Based on Molecular Genetics and lmmunopathology
- Perspective on Melanoma in the Arab World:A Quantitative and Qualitative PubMed-Based Analysis of Research Output (2004–2019)
- Laboratory Safety of Dupilumab, and lts Effect on lnflammatory Biomarkers, in Chinese Adults With Moderate-to-Severe Atopic Dermatitis: An Analysis of a Randomized, Double-Blind Phase lll Study
- Perceptions of Acne and Its Treatments Among Chinese College Students: A Cross-Sectional Survey