Hydromassage of macular hole edges for large and persistent full-thickness macular holes
Yi Cai, Wen-Bo Liu, Duo Wei, Xun Deng, Xiao-Xin Li,5, Ming-Wei Zhao,Xuan Shi, Jian-Hong Liang
1Department of Ophthalmology, Peking University People’s Hospital, Beijing 100044, China
2Eye Diseases and Optometry Institute, Beijing 100044, China 3Beijing Key Laboratory of Diagnosis and Therapy of Retinal and Choroid Diseases, Beijing 100044, China
4College of Optometry, Peking University Health Science Center, Beijing 100044, China
5Xiamen Eye Center of Xiamen University, Xiamen 361102,Fujian Province, China
6Department of Ophthalmology, the Second Hospital of Lanzhou University, Lanzhou 730030, Gansu Province, China
Abstract
● KEYWORDS: macular hole; large macular hole;persistent macular hole; optical coherence tomography;surgical technique; hydromassage
INTRODUCTION
Full-thickness macular hole (MH) is an entity of macular disease defined as a complete defect of neurosensory retinal tissue and could lead to significant vision impairment.The most common type of MH is primary, which is caused by the vitreous-retina separation and traction in anteroposterior or tangential directions on the foveal center.In 1991, Kelly and
Wendel[1]first reported that vitrectomy could treat MH with a success rate of 58%.In 1998, another milestone was achieved by Olenet al[2], who reported that the inner limiting membrane(ILM) peeling in vitrectomy could further enhance the success rate to around 90%, which had reminded all the investigators of the importance of ILM in the mechanism of the disease.With the current standards of MH repair containing threeport trocar placement (23, 25, or 27 gauge), core vitrectomy,creation of posterior hyaloid separation, peripheral vitrectomy,staining, ILM peeling, fluid-air exchange, and gas tamponade, the closure rate of a primary MH had exceeded 90% at present[3].
Nevertheless, a proportion of patients still suffer from incomplete closure of the MH.In complex cases with multiple risk factors, the success rate of the procedure might be compromised.According to Stecet al[4], the closure rate was related to the preoperative diameter of the holes in chronic cases, and MH larger than 400 μm were less likely to close after a standard pars plana vitrectomy (PPV).Recurrent MH with a history of the previous vitrectomy may also be recalcitrant.According to a study by Valldeperas and Wonget al[5]in 2008, the success rate of reoperation within 2mo of the first surgery after failed MH surgery was only 74%.In this way, various adjunctive maneuvers and agents have begun to be investigated in surgery to improve closure rates, although the effectiveness of some of them may still be controversial.In this study, we introduced a new surgical technique namely MH hydrodynamic massage, performed simultaneously with conventional vitrectomy and ILM stripping.It takes up very little time and can deepen our understanding of MH treatment and surgery, especially in refractory cases.
SUBJECTS AND METHODS
Ethical ApprovalThe study complies with the tenets of the Declaration of Helsinki revised in 2013.The study was reviewed and approved by Medical Ethics Committee of Peking University People’s Hospital.All the patients recruited signed the informed consent.
ParticipantsThis is an uncontrolled retrospective study involving a total of 17 eyes from 16 consecutive patients who were diagnosed with refractory or primary large MH at University People’s Hospital Eye Center from 2018 to 2023.The inclusion criteria were as followed: all recruited cases have confirmed the diagnosis of full-thickness MH using spectral domain-optical coherence tomography (OCT) at present or before their first MH repair surgery, with an MH aperture diameter larger than 600 μm on OCT or remained an unclosed MH larger than 600 μm after the last vitrectomy.Cases meeting the following criteria were excluded: 1) high myopia,defined as <-6.00 diopter, or with an axial length (AL) larger than 26.5 mm; 2) secondary to or combined with trauma or other ocular diseases; 3) with an increased intraocular pressure(IOP) at baseline or had a history of glaucoma; 4) poor OCT signals secondary to the reduced refractive interstitial opacity;5) previous intraocular surgery except for the first MH repair surgery within 6mo; 6) Combined with uveitis or scleritis.
If the preoperative MH diameter was greater than 800 μm,it would be classified into “the very large hole group”; the remaining eyes with a preoperative diameter ranged from 600 to 800 μm were categorized as “the large group”, accordingly.Moreover, all cases with a duration of symptoms of more than 2y would be analyzed separately as another subgroup called“the chronic group”, whereas the remains were defined as “the non-chronic group”.Cases with a previous ordinary MH repair surgery were defined as persistent MH.
Surgical ProceduresAll cases received standard threeport vitrectomies (25 gauge), which were performed by one experienced doctor (Liang JH).For those phakic eyes with significant cataracts, phacoemulsification and intraocular lens implant were also combined.Followed by core vitrectomy,a posterior vitreous detachment was made to ensure that the posterior hyaloid was removed entirely.Minimum 2 papillary-diameter (PD) ILM was peeled with the assistant of indocyanine green staining (ICG; approximately 0.2 mL ICG diluted in 5% glucose, which was 1 mg/mL solution).For those who already received a previous MH repair surgery, the range of ILM peeling was extended to 4 PD.Then by using the soft-tip flute needle to massage the hole margin, which is meant to blow and suck gently, to make the retina tissue at the edge of the hole loose and soft through the water flow, thereby creating undulating waves in the hole margin that follow the water’s course.Next, make the edges of the hole approximated as far as possible when absorbing with the flute needle.Sulfur hexafluoride (SF6; 20%) or hexafluoroethane (C2F6; 20%) were applied for gas tamponade followed by complete gas-fluid exchange.Finally, patients recruited were asked to maintain a face-down position for one week postoperatively (Video 1,online supplementary).
Main Outcome MeasuresAll cases received comprehensive assessment before and after the surgery.Baseline characteristics,including the patient’s age, sex, duration of symptoms, AL,spherical equivalence (SE), lens status, and vitrectomy history,were recorded.The preoperative and postoperative anatomic parameters of the MH were measured using two-dimensional spectral-domain OCT (Optovue, Fremont, CA, US), with the standardized 0°, 45°, 90°, 135° sections through the center of macula, which were routinely collected at baseline and every follow-up timepoint.The anatomic quantitative data were obtained from built-in processing software.The following variables were gathered at baseline, 1wk, 1, and 3mo, latest follow-up time after surgery, including best-corrected visual acuity (BCVA), the central retinal thickness (CRT), the length of the bare retina and retinal pigment epithelium (RPE) band,the diameter of the ellipsoid zone (EZ) defect.All parameters were measured by one investigator (Cai Y) 3 times, and the mean values were calculated respectively.
After surgery, the morphological closure type of the MH was classified according to the contour of the macula.A complete hole closure, defined as a complete sealing of the RPE layer without any RPE bared, was classified into type 1 closure.When the MH was closed with a bare RPE section remained but absent of any detachment of the edge, it would be classified as a type 2 closure.An unclosed hole with the rim detached was regarded as a failure of the surgery and would be classified as a type 3 closure[6].
Statistical AnalysisStatistical analyses were performed with SPSS Version 25.0 (SPSS, Inc, Chicago, IL, USA).The BCVA was recorded in decimal units, and then converted to the logarithm of the minimal angle of resolution (logMAR).The descriptive data with normal distribution are presented as the means±standard deviations (range).The comparisons of variables between different closure types were performed by independent samplest-test, and the paired samples two-tailedt-test were undertaken to determine differences before and after surgery.Data that did not demonstrate a normal distribution,such as the age, duration of the symptoms, SE, were expressed as median (interquartile range) and was performed using Mann-WhitneyUtest.Categorical data were expressed asn(%).Differences in categorized data were assessed using Chisquared tests.In multivariate regression models, variables like age, duration of symptom, preoperative lens status, choice of tamponade, SE, and preoperative visual acuity (VA) were selected for analysis, and forward was used in the selection of independent variables.APvalue <0.05 was considered significant.
RESULTS
Totally 17 eyes in 16 patients with the MH aperture diameter larger than 600 μm were enrolled in this retrospective research.Detailed baseline characteristics were presented in Table 1.The 12 (70.6%) cases had a history of a failed MH repair surgery.About the preoperative lens status, there were 7 phakic eyes (41.2%), and during the surgery, 6 of them underwent combined phacoemulsification with intraocular lens implantation.
All eyes enrolled were classified as stage IV MH preoperatively.The overall mean preoperative aperture diameter was 747±156(611, 1180) μm, and the mean base diameter was 1400±413(678, 2220) μm.The aperture and base diameter did not differ significantly between the chronic group and the non-chronic group.The overall mean preoperative VA was 0.99±0.23(range 0.7-1.5) logMAR.There was no statistically significant difference detected between the very large group and the large group (P=0.17), neither between the chronic group and nonchronic group (P=0.10; Table 2).
After surgery, all the cases received a complete anatomical closure of the MH with whether a type 1 (13/17, 76.5%)or type 2 (4/17, 23.5%) closure.There was no significant difference in preoperative OCT variables between type 1 and type 2 closure (Table 3).Cases with a type 2 closure have a longer mean EZ defect compared with cases with a type 1 closure at the 3-month follow-up point after surgery, but no significance was noted (P=0.825).
Totally 14 (82.3%) eyes received statistically significant vision improvement 3mo after the operation, which was achieved in 12/13 (92.3%) of the very large group, and 11/13 (84.6%)of the chronic group.Six (35.3%) cases achieved a gain in VA of more than 2 lines, which was achieved in 0/13 of the very large group and 0/13 of the chronic group.In the nonchronic group and very large group, VA improved significantly after the surgery (P=0.041,P=0.002, respectively).However,between the very large group and large group, visual outcomes(including preoperative and postoperative mean VA and gain in VA) did not differ significantly.In comparing the non-chronic group to the chronic group, there was a significant difference in the gain in VA.The non-chronic group exhibited a substantial gain in VA (-0.30±0.20, range -0.70 to 0), while the chronic group showed a smaller change (-0.05±0.06, range -0.10 to 0,P=0.001; Table 2).

Table 1 Characteristics of subjects and surgical variables
When considering closure types on OCT, eyes with a type 1 closure demonstrated significantly better postoperative VA(0.70±0.10, range 0.50 to 0.80) compared to those with a type 2 closure (0.90±0.12, range 0.80 to 1.00;P=0.03).However,the gain in VA did not differ between the two closure types(P=0.726).Moreover, cases with combined emulsification did not show significant differences in closure type (P=0.978), gain in VA (P=0.219), and EZ defect length (P=0.574) compared to the rest of the cases.The detailed results are presented in Table 3 and Figure 1.OCT images of two cases are illustrated in Figure 2.
DISCUSSION
Although conventional vitrectomy with ILM peeling has been shown to be effective in the treatment of MH, 20% to 60% of large full-thickness MHs still failed to close, and the success of achieving anatomical closure will greatly affect visual outcome[4,7-9].In this way, it remains a challenge to effectively close the hole.Smiddyet al[10]described the use of transforming growth factor-2 as an adhesive to assist in the closure of the MH.Analogously, autologous serum,platelets have been introduced into the procedure afterward[11].Materials similar to the ILM for providing a bridge for the proliferation of glial cells are also used as filler, including auto-transplantation of the anterior lens capsule[12]and human amniotic membrane[13].Adjunctive maneuvers to manipulate the retinal surface have also been proposed, including the inverted ILM peeling technique, defined as creating an incomplete peeling of ILM on macula and invertedly covering the flap over the hole[14]; tapping of MH edges reported by Kumaret al[15]; enlargement of the ILM peeling area and even changing the choice of tamponade[3],etc.

Table 2 Comparison of OCT parameters and preoperative visual acuity mean±SD (range)
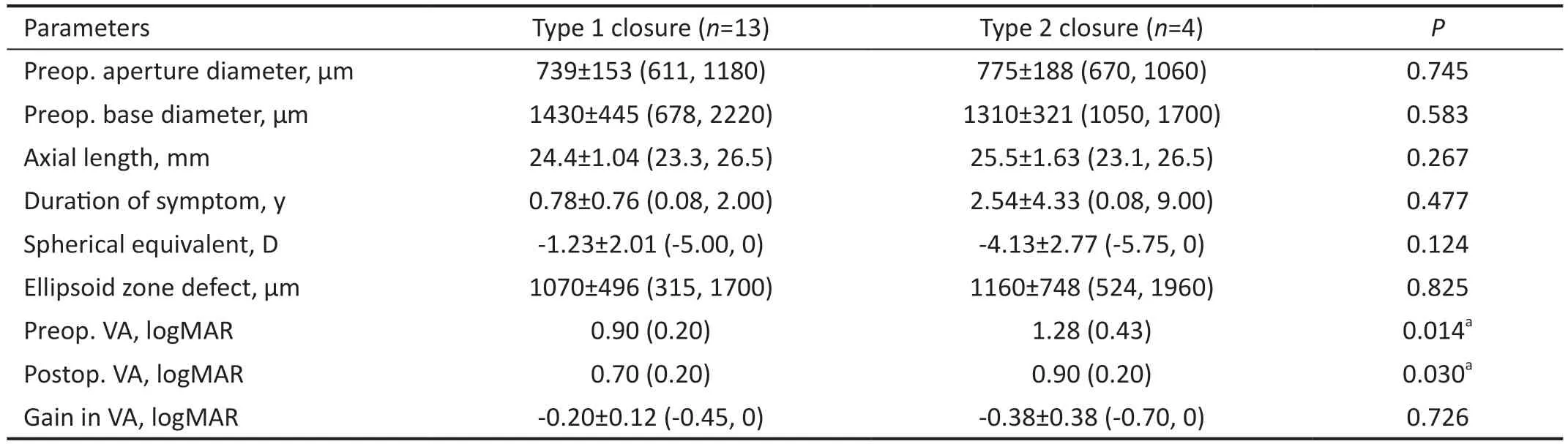
Table 3 The comparison of the characteristics, OCT variables, and visual outcomes between MH with type 1 and type 2 closure

Figure 1 Visual outcomes between cases with type 1 and type 2 closure The preoperative and postoperative VA differed significantly between the 2 groups (P=0.014, P=0.030, respectively).The gain in VA did not show any significant difference between the 2 groups(P=0.726).Cases with type 1 closure received a significantly improved VA after macular hole repair surgery, however in cases with type 2 closure, no such significance was observed (P=0.001, P=0.347,respectively).VA: Visual acuity.
For refractory recurrent holes, hydraulic centripetal macular displacement[16], autologous retinal transplant[17], or induced macular detachment[18]can also be a trial option.
In this study, we presented a novel adjunctive maneuver for large or refractory MH repair procedures.It features using a water stream to assist in softening stiff and puckered hole margins to induce MH margin closure.Its efficacy has been demonstrated both anatomically and functionally: Successful closure was obtained in all cases in this study without any edge detachment, and the overall VA was significantly improved compared to the preoperative VA.Furthermore, 14/17 (82.3%)patients received vision improvement, and 6/17 (35.2%)patients had significantly improved VA by more than 2 lines,especially for eyes with symptoms lasting less than two years.This is in consistency with various previous researches for chronic holes, which are characterized by atrophy of retinal tissue at the MH margin or RPE, and with small increase in VA after MH repair surgery[19-20].

Figure 2 Preoperative and postoperative OCT images of 2 representative cases that underwent the MH repair surgery with the intended hydromassage technique Case 1: Sequential Spectral-domain OCT images of a large primary MH of a 41-year-old man were taken at baseline and three months after the surgery.The preoperative OCT image shows the aperture diameter was 702 μm, and the base diameter was 1090.33 μm (A).The postoperative OCT image shows a type 1 closure achieved after surgery, and central retinal thickness of 75 μm (B).The postoperative VA elevated to 0.6 logMAR 3mo after the surgical repair.Case 2: Preoperative OCT of a large primary MH of a 67-year-old man with an aperture diameter of 670.21 μm, the basal diameter of 1064.76 μm (C).Preoperative VA was 1.0 logMAR.Postoperative OCT showing type 2 closure, with a section of bare RPE, remained three months after the surgery (D).His VA was elevated to 0.8 logMAR, three months after the surgery.E, F: Screenshot for hydromassage technique: use the soft-tip flute needle to massage the hole margin, and to blow and suck gently, making the retina tissue at the edge loose and softthrough the water flow.Second, make the edges of the hole approximated as far as possible when absorbing with the flute needle.OCT: Optical coherence tomography; MH: Macular hole; VA: Visual acuity; RPE: Retinal pigment epithelium.
Although there were many factors related to the postoperative visual outcomes, including aperture/basal diameter of the hole, previous failed PPV history, chronicity,etc., the contour of the closure was deemed as a significantly relevant factor.According to previous research[21], the postoperative hole closure on OCT was divided into two types according to the morphology.This was a more distinct classification rather than the previous classification system of U type and V type introduced by Imaiet al[22], which was ambiguous in the definition to some extent.In this way, we adopted the former classification system in our analysis.It was noted that postoperative VA was highly associated with the contour of the closure.Patients with a type 1 closure had a significantly better postoperative VA compared with cases with a type 2 closure,which is consistent with the previous research[6].
In order to create a type 1 closure with neuroretina restoration,gliosis proliferation, and especially glial cell photoreceptor layer reconstruction on the bare RPE layer[23], As mentioned above, a combination of traditional vitrectomy and a number of adjuncts has been widely used.There were roughly two groups of additive surgical techniques according to the principle: the first group was the plug or elongation of the tissue, including the usage of autologous gluconated blood[24], autologous platelets[11,25], and inverted ILM flap technique.These plugs provided the scaffold, muller cell remains, or cytokines for introducing the glial cells and photoreceptors to migrate and proliferate[14].However, many refractory large macular holes had the history of failed vitrectomies and did not have ideal remains to repeat ILM peeling or plugging.Maintaining the location of the flap also requires a degree of surgical skill.Moreover, it was also reported that some chronic MH showed unique morphological characteristics compared with acute MH, such as the squarer, puckered configuration of the margin with stiffness[26].It is also believed that refractory MHs always have a tight, sometimes pigmented retinal-RPE adhesions[27].Besides, according to the hydration theory, the liquid vitreous after vitrectomy surgery might get into the margin of MH and would be absorbed by the retinal layers evidence by OCT: the inner retinal layers could get retracted away from each other,and the swelling of the middle and outer retinal layers could cause an increase in base diameter of the hole.Therefore,another key factor for hole closure is isolating the hole from vitreous fluid either by intraocular tamponade or mechanical approximating, which facilitates the functional recovery of the RPE pump[28].The situations mentioned above could not be solved simply by a plug or elongation.So another group of mechanical maneuvers characterized by lysing the adhesion with RPE, enhancing the retinal compliance, reducing the intrinsic retinal stiffness, thus helping the margin to involute and proximate emerged were proposed, as the technique of tapping the edges of MH[15], iatrogenically creating a limited macular detachment introduced by Claes[29], MH hydro-dissection technique (MHH) proposed by Felfeli and Mandelcorn[30], and hydraulic centripetal macular displacement reported by Rubanet al[16].Our study belonged to the latter group too.It is a safe way of helping reduce the stiffness of the margin and avoid harming the underlying RPE cells at the same time.As shown in our study, the 100% closure rate was indeed achieved.We speculate that it could be analogous to a soft massage through the water flow, which moves the edges and increases flexibility without unnecessary mechanical damage.In this aspect, it is consistent with the MHH technique proposed by Felfeli and Mandelcorn[27].Both techniques help to elevate the mobilization of MH edges, allowing them to reapproximate.And our way of soft massage is not intended to process with the mechanical dissection of the retina, so it will reduce the mechanical damage directly towards the retina during water injecting manipulation and minimize the trauma to the RPE.
In our research, 4 eyes achieving type 2 closure (4/17, 23.5%).However, they did not have a significantly larger aperture/basal diameter or longer duration of symptoms compared with other eyes.There may be various factors contributing to it[30].Among them, the incomplete separation of adhesions may be one of the most important.According to Ishidaet al[31], the displacement of the retina around the MH was frequently observed by studying the displacement of the vessels, and the extent of the displacement may be related to the extent of the detachment of the macula.In this situation,the combination with the MHH technique/hydraulic centripetal macular displacement technique mentioned above may have an added value[16,27].They can add the volume of the margin tissue through hydration, help to extend the hole margins through the injection of the fluid under the retina, and more adequately alleviate the adhesion around the MH margin at the same time[27].Therefore, in those recalcitrant large holes with a dislocation adhesion, simply soft massage may be limited effective, a combined hydro-dissection, even iatrogenic limited macular detachment might address the problem.
The advantage of our research is that the manipulate is repeatable and straightforward, with limited damage, and needs less time or practice compared with other types of surgical techniques.It only needs a little time gently massaging the margin of the hole through water flow, in this way it can make the hole edges more compliant, which is favorable in introducing the hole margin proximate.The limitations of our research are that the sample size is too small, and there was no control group designed for comparing the distinct difference,the single non-masked observational nature restricted its conviction.Another weak point is the large variability in follow-up duration.Besides, we only use VA and EZ injury to evaluate the potential damage might cause by the procedure.We will employ various methods in the future to assess the structural and functional impacts resulting from MH surgery.Further, carefully designed clinical experiments and larger study groups remain to be constructed to estimate the validity of this technique.
The MH hydromassage technique could provide an acceptable closure rate in large holes or persistent MH cases.It needs less time and practice, with little damage to the retina tissue and RPE.It may become a preferred adjunct to the MH repair surgery.
ACKNOWLEDGEMENTS
Authors’ contributions:Liang JH, Li XX, Shi X defined the criteria for inclusion and exclusion.Liang JH performed all the vitrectomy surgery.Wei D, Cai Y, Shi X analyzed and interpreted the patient data, Wei D, Cai Y, Liu WB drafted this manuscript, Deng X and Wei D made the figures and tables.Shi X, Deng X, Li XX, Liang JH, Zhao MW modified the manuscript.All authors read and approved the final manuscript.
Foundation:Supported by National Natural Science Foundation of China (NSFC) fund (No.81970815).
Conflicts of Interest:Cai Y,None;Liu WB,None;Wei D,None;Deng X,None;Li XX,None;Zhao MW,None;Shi X,None;Liang JH,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Meibomian glands segmentation in infrared images with limited annotation
- Artificial intelligence for the detection of glaucoma with SD-OCT images: a systematic review and Meta-analysis
- Overexpression of TRPV1 activates autophagy in human lens epithelial cells under hyperosmotic stress through Ca2+-dependent AMPK/mTOR pathway
- Dry environment on the expression of lacrimal gland S100A9, Anxa1, and Clu in rats via proteomics
- Semaphorin 7A impairs barrier function in cultured human corneal epithelial cells in a manner dependent on nuclear factor-kappa B
- Novel MIP gene mutation causes autosomal-dominant congenital cataract
