Effect of navigation endoscopy combined with threedimensional printing technology in the treatment of orbital blowout fractures
Jin-Hai Yu, Yao-Hua Wang, Qi-Hua Xu, Chao Xiong, An-An Wang, Hong-Fei Liao
1School of Optometry, Jiangxi Medical College, Nanchang University, Nanchang 330006, Jiangxi Province, China
2The Affiliated Eye Hospital, Jiangxi Medical College,Nanchang University, Nanchang 330006, Jiangxi Province,China
3Jiangxi Clinical Research Center for Ophthalmic Disease,Nanchang 330006, Jiangxi Province, China
4Jiangxi Research Institute of Ophthalmology and Visual Science, Nanchang 330006, Jiangxi Province, China
5Jiangxi Provincial Key Laboratory for Ophthalmology,Nanchang 330006, Jiangxi Province, China
Abstract
● KEYWORDS: orbital blowout fracture; three-dimensional printing; endoscopy; surgical navigation
INTRODUCTION
Due to the rapid development of technology and economy, the incidence of orbital fractures caused by traffic accidents and industrial production accidents has been increasing year by year.The orbital cavity of the human body is formed by seven bones and roughly resembles a quadrangular pyramid in shape.The orbital bone wall consists of an inner wall, inferior wall, lateral wall, and roof wall.The inner wall and inferior wall, being thin, are more susceptible to fractures[1].Orbital fractures can be classified into two types: simple and compound.Simple fractures are characterized by the fracture being confined to one or more orbital walls, also referred to as blowout fractures.Compound fractures involve both the orbital wall and the orbital rim.The current understanding of the mechanisms underlying orbital fractures mainly involves the theories of intraorbital fluid pressure and orbital force conduction[2-4].The orbital bone contains numerous foramina and fissures through which important nerves and blood vessels pass to regulate the normal physiological functions of the eyeball.Consequently,orbital fractures can result in symptoms such as diplopia, eye movement disorder, enophthalmos, and sensory disturbances,significantly impacting the patients’ short-term quality of life[5].Treatment options for orbital fractures primarily consist of conservative and surgical approaches.However, there is currently no internationally agreed-upon consensus regarding the indications for surgical intervention[6-7].In our opinion,initial-stage orbital fractures can be managed using medication and eye movement training.Surgical intervention should be considered in cases where the patient experiences persistent diplopia symptoms or when imaging reveals extensive soft tissue herniation into the paranasal sinuses within the orbit.The surgical outcome of orbital fractures is predominantly influenced by the surgeon’s clinical expertise and surgical proficiency.Common complications following orbital fractures include eyelid retraction, persistent diplopia, orbital hematoma,and orbital cyst formation[8-9].The occurrence of complications can further deteriorate the patient’s quality of life.
This study aims to compare the efficacy of traditional surgery with that of surgical navigation, nasal endoscopy combined with 3D printing technology (3DPT) in the treatment of orbital blowout fractures (OBF).The specific objectives of this study are to compare the duration of the operation, best corrected visual acuity (BCVA), enophthalmos difference, recovery rate of eye movement disorder, recovery rate of diplopia, and incidence of postoperative complications between the two groups, aiming to evaluate the differences in efficacy.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Medical Ethics Committee of the Affiliated Eye Hospital of Nanchang University (Protocol No.YLP20221002), and it was conducted in accordance with the principles outlined in the Declaration of Helsinki.
Study Design and SampleIn order to achieve the research objectives, we conducted a retrospective cohort study.The study included patients with orbital fractures who were admitted to the Affiliated Eye Hospital of Nanchang University and underwent surgical treatment between July 2012 and November 2022.Inclusion criteria for the research sample were as follows: all patients were operated on by the same chief physician; the patients’ clinical data were complete,and they were followed up for a minimum of 6mo.Patients meeting any of the following criteria were excluded from the study: orbital rim fractures or eyeball rupture; fractures in both eyes simultaneously; fractures that had undergone surgical treatment for more than 6mo.All patients provided informed consent prior to the operation.
Design and Production of Orbital 3D ModelAll patients in the new surgical group underwent a preoperative orbital computed tomography (CT) scan with a slice thickness of 0.6 mm.Save the acquired Digital Imaging and Communication in Medicine (DICOM) file data to a CD.Mimics 21.0 software (Materialise, Belgium) was utilized to determine the bone threshold value from the DICOM data imported from the CD.Subsequently, the “Region Grow” commands were executed to reconstruct the 3D model.The reconstructed data of the orbital fracture model were saved in the stereolithography (STL) file format and imported into the reverse engineering software, Geomagic Studio 12.0 (Geomagic Corporation, USA).The software mirrors the orbital model from the healthy side to the affected side, creating a prosthetic model.Employ the “Curve Cut”command to delineate the fracture area, and utilize the “Shell”command to design a surgical guide that aligns with the anatomical shape of the bone defect region.The designed guide plate and orbital fracture model data were imported into a Form2 printer (KONICA MINOLTA, Japan) for 3D printing.The printed model and guide plate undergo cleaning, drying,and low-temperature plasma sterilization for subsequent use.
Preparation of Surgical Navigation System and Nasal Endoscopy SystemImport the CT data of patients in the new surgical group into the Medtronic Navigator workstation(Medtronic, USA).Position the dynamic reference frame near the patient’s orbit and perform fusion registration of the periorbital facial skin using the probe tracer and positioning detection system.This aligns the spatial coordinate system of the image data with the actual spatial coordinate system.Verify that each system is functioning properly to ensure accurate intraoperative positioning and navigation.All patients in the new surgical group underwent surgery with the assistance of a nasal endoscope (STORZ KARL company, Germany).Prior to the procedure, power on the split main unit, which includes the cold light source, video camera, and display.Connect the endoscopic probe and thoroughly debug each system to ensure it is in a functional state, enabling visual operation during the procedure.
Surgical ProcedurePrior to the procedure, antibiotics are administered to prevent infection, and the operation is conducted under general anesthesia.Select an appropriate surgical approach based on the location and extent of the fracture, which may include the conjunctival approach, skin approach, or a combination of both.In the new surgical group,the surgical navigation system was employed to identify the periosteal separation process in real-time, thus minimizing the risk of damaging vital nerves and blood vessels within the orbit.Simultaneously, the fracture edge was visualized using an endoscope, allowing for the release of incarcerated soft tissue and addressing any herniated soft tissue into the paranasal sinus (Figure 1).The fracture repair material was shaped based on the surgical guide, and the model was utilized for validation to achieve anatomical repair of the orbital wall defect (Figure 2).In the control group, orbital wall defects were repaired using traditional surgical techniques.The periosteum was sutured with 5-0 sutures, while the skin or conjunctival incision was closed with 6-0 sutures.Postoperatively, antibiotics were administered to prevent infection, and glucocorticoids were utilized for anti-inflammatory purposes.Extraocular muscle function training commenced on the 3rdday following the operation.
Data Collection MethodsPatients were tested for the following indicators 1d before the operation and at 1wk, 1,and 3mo post-operation.The international standard eye chart is used to measure the BCVA.The Hertel exophthalmometer is used to measure enophthalmos and calculate the difference between the normal and affected eyes.Diplopia is assessed using the Hess screen and red glass test.Eye movement disorder is assessed using the synoptophore and nine-direction test.Diplopia is classified into the following grades: Grade 0 indicates no diplopia; Grade I indicates no diplopia when looking straight ahead, but diplopia in the peripheral vision;Grade II indicates diplopia when looking straight ahead and in 1 peripheral quadrant; Grade III indicates diplopia in multiple quadrants directly in front of the gaze and in the periphery.Eye movement disorder are classified according to Nagyet al’s[10]criteria into the following grades: Grade 0 indicates no restriction of eye movement; Grade I indicates limited movement in one or more directions; Grade II indicates significant limitation of motion in one or more directions;Grade III indicates movement in one or more directions beyond the midline position is not possible.Recovery to grade 0 of postoperative diplopia and eye movement disorder was defined as returning to a normal state.All patients were followed up for a minimum of 6mo, and the type and number of complications were documented.
Statistical AnalysisThe data analysis was performed using SPSS 23.0 statistical software (IBM Corporation, USA).In this study, the duration of the operation, BCVA, and other measurement data were reported as mean±standard deviation(SD), and analyzed using the Student’st-test.The recovery rates of postoperative eye movement disorder and diplopia, as well as the incidence of complications, were compared using the Chi-square test for count data.Dichotomous data were analyzed using odds ratio (OR) as the effect size, accompanied by 95% confidence interval (CI).The difference in enophthalmos parameters did not follow a normal distribution and was reported as median (range).The non-parametric Wilcoxon signed-rank test was employed.A difference was considered statistically significant if theP-value was less than 0.05.
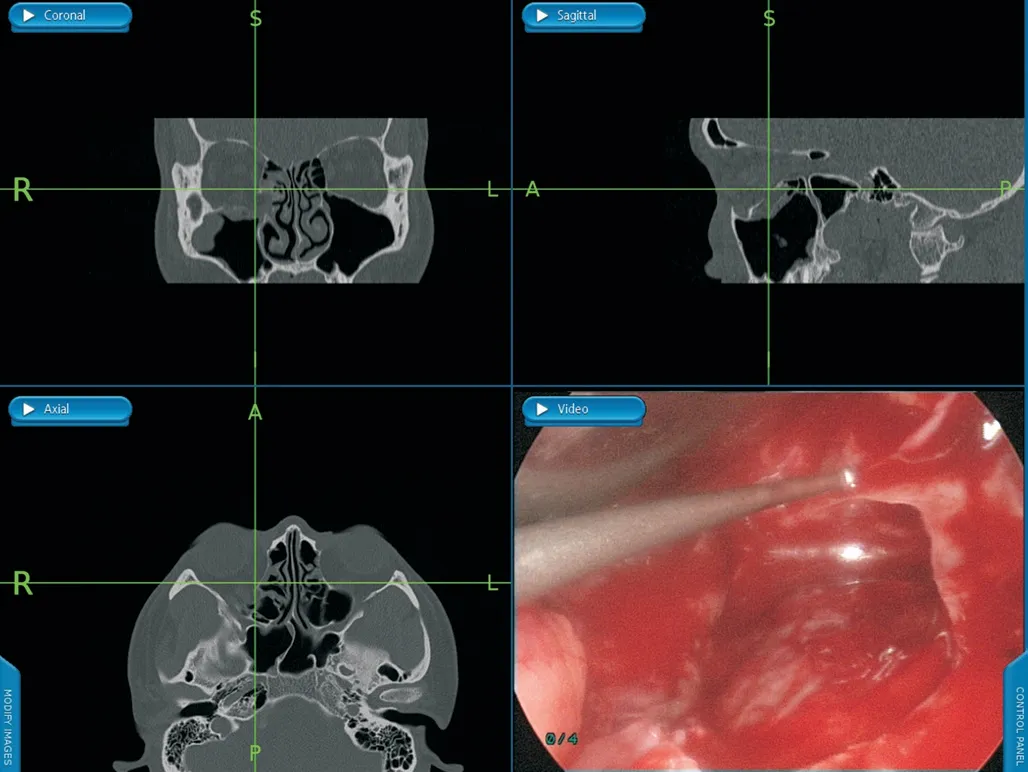
Figure 1 The utilization of a surgical navigation system and endoscope-assisted dissection for incarcerated soft tissue in the area of an orbital wall defect.
RESULTS
Basic Information of the Selected PatientsThe study included a total of 95 cases with 95 eyes (37 cases in the right eye and 58 cases in the left eye).The study population consisted of 63 males and 32 females, ranging in age from 5 to 67y, with a mean age of 35.21±15.75y.The control group consisted of 43 cases, while the new surgical group consisted of 52 cases.The causes of injury included car accidents, falls,assault, and other accidents.The time interval between injury and operation ranged from 2 to 125d, with a mean duration of 18.25±19.98d.The postoperative follow-up period ranged from 6 to 24mo.Statistical analysis showed no statistically significant differences in baseline demographic characteristics and fracture locations between the control and new surgical groups (Table 1).
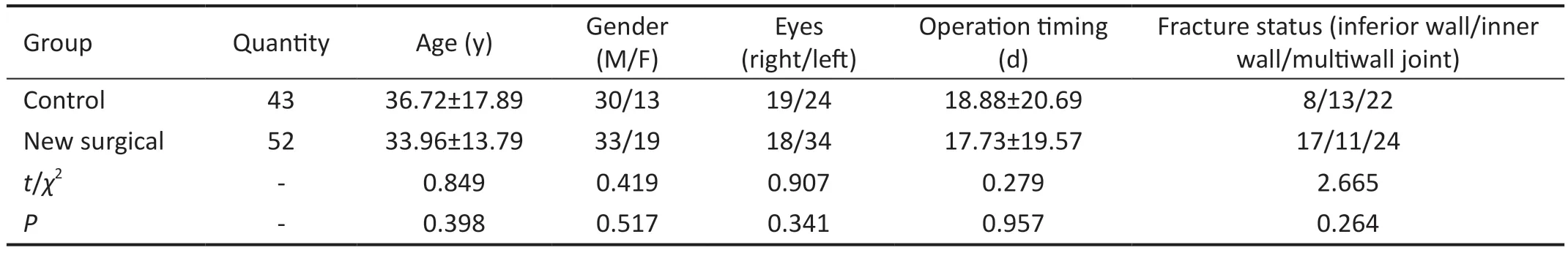
Table 1 Baseline demographic characteristics and fracture location of patients in the 2 groups
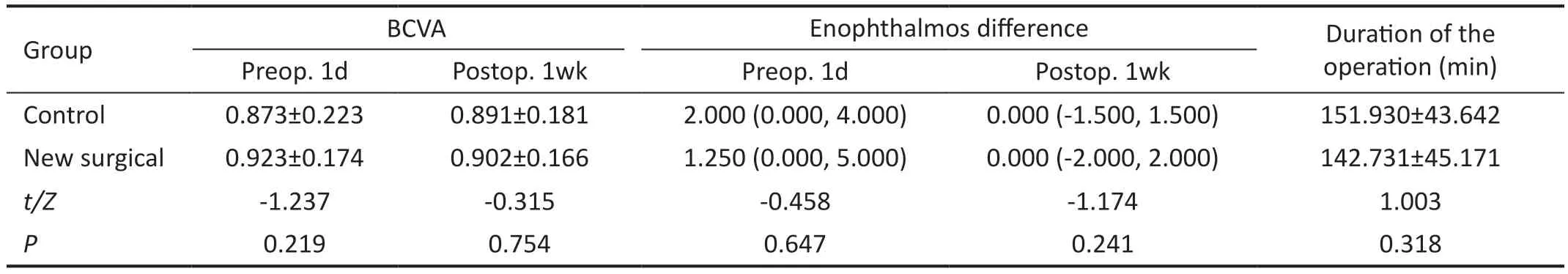
Table 2 The duration of the operation, BCVA, enophthalmos difference between the control group and the new surgical group
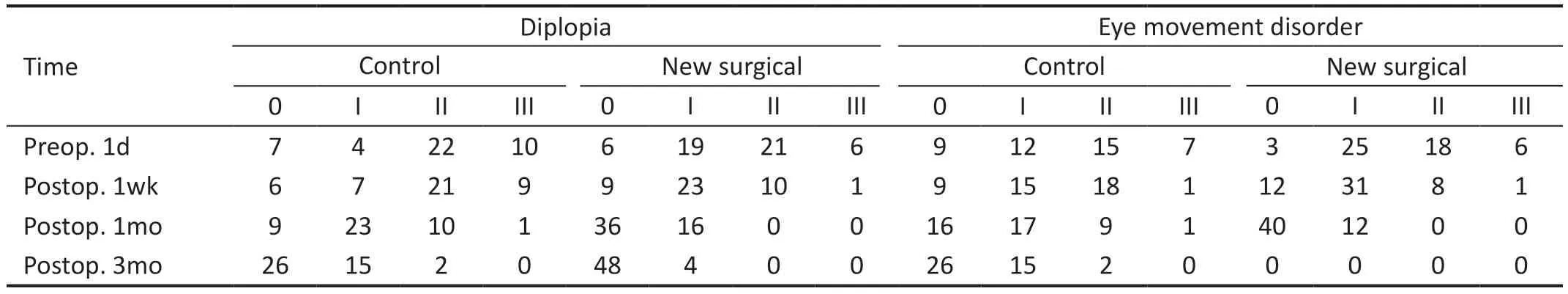
Table 3 Diplopia and eye movement disorder in the control and new surgical groups
Duration of the Operation, BCVA and Enophthalmos Difference of Patients in the Two GroupsThe data indicated that there were no statistically significant differences in the duration of the operation, BCVA, enophthalmos difference between the two groups at 1d before the operation and 1wk after the operation (Table 2).
Recovery of Diplopia and Eye Movement Disorder in the Two GroupsIn the control group, 36 patients had varying degrees of diplopia before the operation.At 1mo after the operation, 2 patients recovered from diplopia, and at 3mo after the operation, 19 patients recovered from diplopia.In the new surgical group, 46 patients had varying degrees of diplopia before the operation.At 1mo after the operation, 30 patients recovered from diplopia, and at 3mo after the operation, 42 patients recovered from diplopia.In the control group, a total of 34 patients had varying degrees of eye movement disorder before the surgery.At 1mo after the surgery, 7 patients had normal eye movement, and 3mo after the surgery, 17 patients had normal eye movement.In the new surgical group, a total of 49 patients had varying degrees of eye movement disorder before the surgery.At 1mo after the surgery, 37 patients had normal eye movement, and at 3mo after the surgery, all patients had returned to normal.The data indicates a gradual increase in the number of patients who fully recovered from diplopia and eye movement disorder in both groups at 1 and 3mo after the surgery (Table 3).
Recovery Rate of Eye Movement Disorder, Diplopia Recovery Rate and Incidence of Complications in the Two GroupsThe statistical results indicated a significantly higher recovery rate of diplopia and eye movement disorder in the new surgical group compared to the control group at 1 and 3mo after the operation.The diplopia recovery rate in the new surgical group 1mo post-surgery surpassed that in the control group [OR=0.03, 95%CI (0.01-0.15),P<0.0000].Similarly, the diplopia recovery rate at 3mo after surgery was higher in the new surgical group compared to the control group [OR=0.11,95%CI (0.03-0.36),P<0.0000].Additionally, the recovery rate of movement disorders in the new surgical group at 1mo postsurgery was significantly higher than that in the control group[OR=0.08, 95%CI (0.03-0.24),P<0.0000], and at 3mo postsurgery, it remained higher [OR=0.01, 95%CI (0.00-0.18),P<0.0000].At 6mo after the operation, the control group experienced 7 cases of complications, which included 2 cases of postoperative hematoma, 2 cases of postoperative implant infection, 1 case of lower eyelid retraction, 1 case of epiphora,and 1 case of persistent diplopia.The new surgical group had 2 cases of complications, both of which were persistent diplopia.The incidence of postoperative complications was lower in the new surgical group compared to the control group [OR=4.86,95%CI (0.95-24.78),P<0.05; Table 4].
Preoperative and Postoperative Appearance of the New Surgical GroupOne patient in the new surgical group hadan orbital fracture affecting the inner and inferior walls of the right eye.Before the surgery, the right eye had limited upward and outward rotation, resulting in a 3 mm difference in binocular enophthalmos.One week after the surgery, the right eye movement disorder resolved, and there was no difference in binocular enophthalmos (Figure 3).
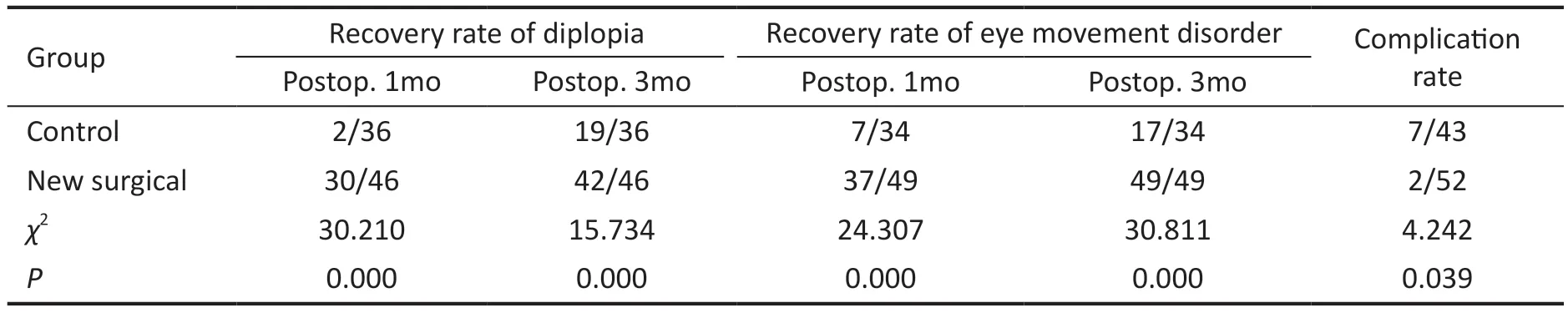
Table 4 The recovery rate of eye movement disorder, diplopia recovery rate and complication rate in the new surgical group and the control group
DISCUSSION
This study aimed to compare the effects of traditional surgery and new technology-assisted surgery in treating OBF.The study revealed a significantly higher recovery rate of binocular diplopia and eye movement disorder symptoms in the new surgical group compared to the control group at 1 and 3mo post-operation.Additionally, the incidence of complications within 6mo post-operation was lower in the new surgical group.Furthermore, the study revealed no statistically significant differences between the two groups in terms of BCVA, enophthalmos difference, or duration of the operation.Additionally, both treatments effectively improved diplopia and eye movement disorder.The purpose of orbital fracture surgery is to address soft tissue incarceration and orbital wall defects.Therefore, it is expected that there would be no impact on the BCVA of both groups.Both groups showed effective improvement in eye-related symptoms, indicating that surgical treatment successfully achieved its intended outcome.The absence of statistical difference in the duration of the operation between the two groups may be attributed to the fact that while the new surgical group saved time in the placement of prosthetic materials, it also required additional time for the preparation and utilization of surgical navigation and endoscopy.

Figure 3 Eye movement and enophthalmos before and after operation in the new surgical group.
The surgical navigation system primarily consists of a positioning detection system, a reference frame, a tracer, and a workstation.In the early stages, the navigation system was extensively utilized in neurosurgery-assisted procedures[11].In recent years, orbital surgeons have started utilizing surgical navigation systems in orbital fracture surgery as well[12].The narrow orbital space contains numerous crucial nerves and blood vessels, which are also in close proximity to the paranasal sinuses and cranial fossa.Utilizing the navigation system enables accurate localization of critical anatomical structures, aiding surgeons in minimizing damage to vital tissues during the operation[13].In recent years, endoscopes have gained popularity in minimally invasive ophthalmic surgery due to their excellent visualization capabilities[14].The use of nasal endoscopy in eye and nose-related surgeries is also widespread[15-16], with demonstrated auxiliary benefits in orbital fractures[17].The nasal endoscopy system primarily consists of a light source, camera, image workstation, monitor,and power operation probe[18].It allows for visualized surgical operations in confined spaces.Utilizing the nasal endoscope system in orbital fracture repair helps overcome the limitations of the surgical field.The endoscope aids in clear observation of the fracture area, enabling the operator to minimize damage to protruding soft tissues and avoid harm to vital nerves and blood vessels.The combination of surgical navigation and the nasal endoscopy system enhances the safety of orbital fracture surgery[19].3DPT, also referred to as rapid prototyping technology, is an additive manufacturing process that builds objects layer by layer using materials, based on 3D model data[20].This technique has found extensive applications in the medical field.Orthopedic surgeons utilize this technology to 3D print models of fracture sites, which serve as precise references for preoperative planning, simulated surgeries, and intraoperative guided repairs[21].The orbit consists of multiple bones and is a confined space with numerous vital tissues,including nerves, blood vessels, and extraocular muscles.As a result, orbital fracture repair surgery is challenging, high-risk,and prone to complications.In traditional surgical methods,surgeons rely on careful examination of patient imaging data to estimate the location and extent of the fracture.Based on their experience, they iteratively trim, shape, and adjust the repair materials to achieve successful orbital wall defect repair.Recently, 3DPT has been increasingly employed to support orbital fracture repair surgeries.Studies have demonstrated that 3DPT can enhance the precision of orbital fracture repair surgeries[22].
This study’s strength lies in investigating the impact of combined assistive technologies, including surgical navigation,endoscopy, and 3D printing, on the surgical outcomes of OBF.This complementary technology has enhanced surgical quality in three key aspects: safety, visualization,and precision.The study’s findings revealed that the new surgical group successfully achieved anatomical repair of orbital wall defects within the visualized surgical field.The new surgical group exhibited faster recovery of diplopia and eye movement disorder symptoms and experienced fewer complications compared to the traditional surgery group.One limitation of this study is its retrospective cohort design,which may introduce potential biases related to factors such as age, timing of the operation, and fracture status during the sample selection process.Nevertheless, a lack of statistical difference between the control and new surgical groups when considering these factors ensures the results’ reliability to a significant extent.
This study compared the treatment outcomes between the new surgical and control groups, revealing that the surgical navigation system enables real-time monitoring of the surgical process.With the assistance of the endoscope system, the fracture area can be operated on under direct visualization,minimizing the risk of damaging critical blood vessels and nerves.Furthermore, the utilization of 3DPT enhances the precision of fracture repair[23].The study’s findings revealed that both the control group and the new surgical group achieved effective improvement in diplopia and eye movement disorder symptoms among patients with orbital fractures.However, the new surgical group exhibited a faster recovery and experienced fewer complications.In conclusion, we contend that the utilization of surgical navigation, endoscopic systems, and 3DPT can enhance the safety and precision of orbital blowout fracture repair surgeries while reducing surgical complications.
ACKNOWLEDGEMENTS
Foundation:Supported by the Jiangxi Provincial Natural Science Foundation (No.20232ACB206030).
Conflicts of Interest: Yu JH,None;Wang YH,None;Xu QH,None;Xiong C,None;Wang AA,None;Liao HF,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Meibomian glands segmentation in infrared images with limited annotation
- Artificial intelligence for the detection of glaucoma with SD-OCT images: a systematic review and Meta-analysis
- Overexpression of TRPV1 activates autophagy in human lens epithelial cells under hyperosmotic stress through Ca2+-dependent AMPK/mTOR pathway
- Dry environment on the expression of lacrimal gland S100A9, Anxa1, and Clu in rats via proteomics
- Semaphorin 7A impairs barrier function in cultured human corneal epithelial cells in a manner dependent on nuclear factor-kappa B
- Novel MIP gene mutation causes autosomal-dominant congenital cataract
