Comments by opponents on the British Medical Association’s guidance on non-therapeutic male circumcision of children seem one-sided and may undermine public health
Stephen Moreton,Guy Cox,Mark Sheldon,Stefan A Bailis,Jeffrey D Klausner,Brian J Morris
Stephen Moreton,CircFacts,Warrington WA5 1HY,Cheshire,United Kingdom
Guy Cox,Australian Centre for Microscopy &Microanalysis and School of Aeronautical,Mechanical and Mechatronic Engineering,University of Sydney,Sydney 2006,New South Wales,Australia
Mark Sheldon,Medical Humanities and Bioethics Program,Feinberg School of Medicine,Northwestern University,Chicago,IL 60661,United States
Stefan A Bailis,Cornerstone Therapy &Recovery Center,St.Paul,MN 55101,United States
Jeffrey D Klausner,Department of Medicine,Population and Public Health Sciences,Keck School of Medicine,University of Southern California,Los Angeles,CA 90089,United States
Brian J Morris,School of Medical Sciences,University of Sydney,Sydney 2006,New South Wales,Australia
Abstract The British Medical Association(BMA)guidance on non-therapeutic circumcision(NTMC)of male children is limited to ethical,legal and religious issues.Here we evaluate criticisms of the BMA’s guidance by Lempert et al.While their arguments promoting autonomy and consent might be superficially appealing,their claim of high procedural risks and negligible benefits seem one-sided and contrast with high quality evidence of low risk and lifelong benefits.Extensive literature reviews by the American Academy of Pediatrics and the United States Centers for Disease Control and Prevention in developing evidence-based policies,as well as risk-benefit analyses,have found that the medical benefits of infant NTMC greatly exceed the risks,and there is no reduction in sexual function and pleasure.The BMA’s failure to consider the medical benefits of early childhood NTMC may partly explain why this prophylactic intervention is discouraged in the United Kingdom.The consequence is higher prevalence of preventable infections,adverse medical conditions,suffering and net costs to the UK’s National Health Service for treatment of these.Many of the issues and contradictions in the BMA guidance identified by Lempert et al stem from the BMA’s guidance not being sufficiently evidence-based.Indeed,that document called for a review by others of the medical issues surrounding NTMC.While societal factors apply,ultimately,NTMC can only be justified rationally on scientific,evidence-based grounds.Parents are entitled to an accurate presentation of the medical evidence so that they can make an informed decision.Their decision either for or against NTMC should then be respected.
Key Words: Circumcision,Male;Child;Infections;Risk;Policy;Public health
INTRODUCTION
In 2019 the BMA released practical guidance for doctors on non-therapeutic male circumcision(NTMC)of boys[1].This stated that it “abhors the harassment of individual doctors through intimidating and threatening behaviour on the basis of their involvement in the provision of NTMC”.As with vaccination,NTMC attracts criticism from activists.Opponents argue that NTMC of a nonconsenting child violates their human rights to genital integrity and that circumcision should be delayed until they are old enough to make the decision for themselves.There are,however,sound scientific reasons why early NTMC is beneficial to the child’s health.These include protection against infections in infancy and infections,including sexually transmitted ones,disease and other adverse medical conditions over the lifespan.Reduced risk of penile[2-4] and possibly prostate[5,6] cancer is greatest the earlier the NTMC is performed,being particularly strong(40% lower)in Black men[6].Risk was lower in men circumcised after age 36 years in the Canadian study[6].In the current “post-truth era”,in which individuals and lobby groups dispute scientific evidence by way of on-line rhetoric,threats and intimidation using social media and protests to promote their views,the challenge for scientists and society is considerable[7-15].As with other decisions by parents made in what they consider to be the best interest of the child,such as vaccination,lobbying by opponents can involve inappropriate pressuring of parents to reconsider their decision to have their sons circumcised.
The most recent reviews by the American Academy of Pediatrics(AAP)[16] and the United States(US)Centers for Disease Control and Prevention(CDC)[17] concluded that the health benefits of NTMC exceeded the risks and recommended the procedure for parents who choose it(Table 1).

Table 1 Conclusions and recommendations by the American Academy of Pediatrics in its non-therapeutic male circumcision policy statement
NTMC opponents responded by denouncing the new policies.The claims were evaluated by the AAP,CDC,and academic authorities and found not to be consistent with the consensus of scientific evidence(Table 2).
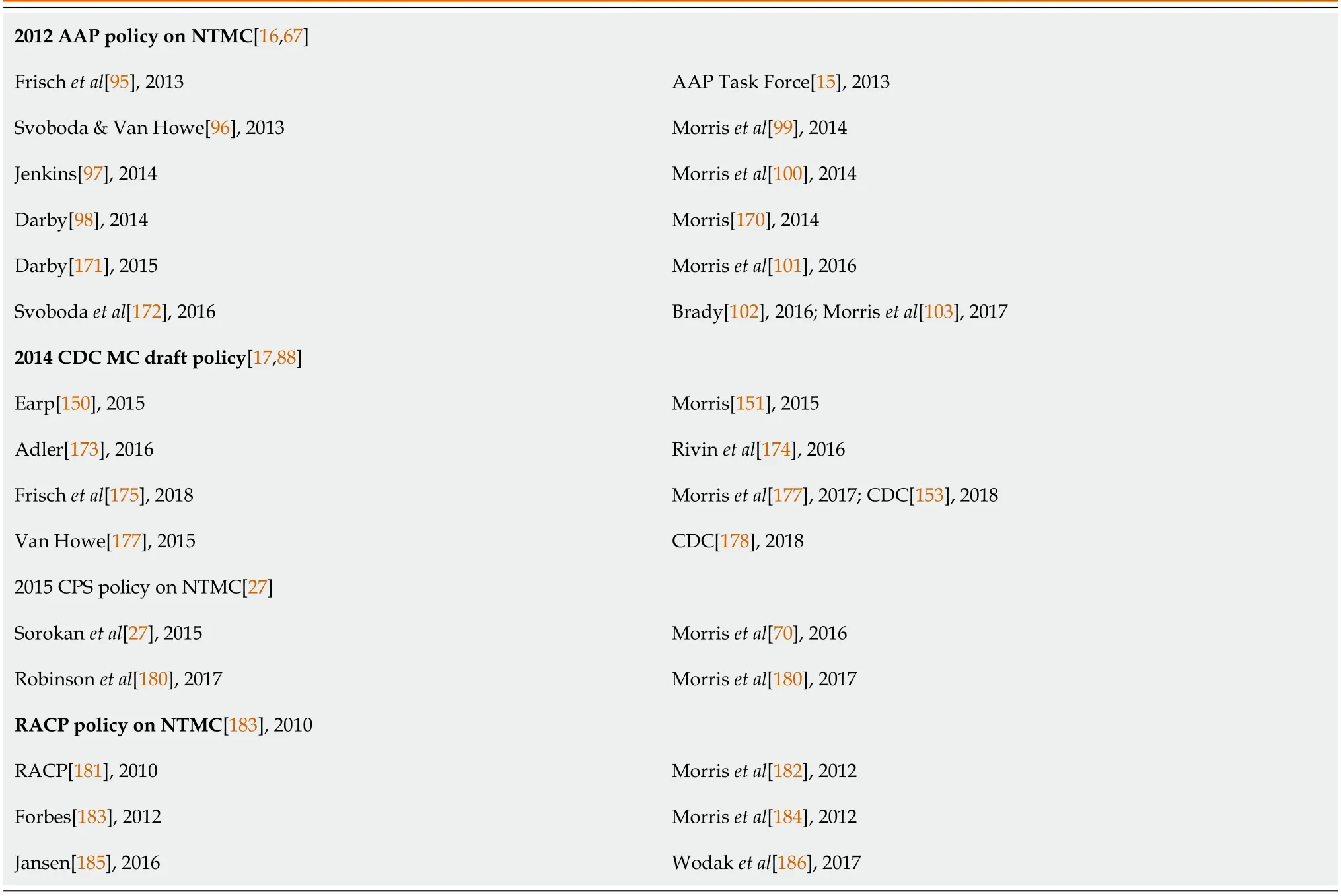
Table 2 Nontherapeutic male circumcision policy statements showing arguments by opponents(left column)and responses to each(right column)
Selective citation,obfuscation and denial of scientific evidence are features of anti-NTMC arguments.Most of these and the evaluation of each publication by medical authorities can be found in a systematic review[18].
The BMA guidance attracted the attention of NTMC opponents Antony Lempert,Chair of the Secular Medical Forum which advises the United Kingdom’s National Secular Society,in an article with ethicist Brian Earp as author for correspondence,and two others[19].The aim of the present article is to evaluate their arguments.
ANTI-NTMC SENTIMENTS BY OTHER MEDICAL BODIES
Lempertetal[19] support particular statements in the BMA’s guidance[1] disfavoring NTMC.They refer to negative NTMC policies by Dutch(Kindermishandeling en huselijk geweld [KNMG]:Royal Dutch Medical Association),Danish and Finish medical bodies.Then refer to the Finnish Medical Association as being “more forward in their approach,offering a clear medical-ethical stance for consideration”.They argue that “mainstream,non-partisan,national-level professional societies that have formally studied the issue”,with the exception of those in the United States,“have concluded that NPC [NTMC] of children cannot be justified on medical grounds in the sense of conferring a net health benefit”.Infant NTMC was endorsed in high human immunodeficiency virus(HIV)settings by various bodies combatting the HIV epidemic.According to a recent editorial[20],however,the World Health Organization(WHO)no longer endorses NTMC of infants in its voluntary medical male circumcision(VMMC)program.Reasons likely include immediate cost-effectiveness of NTMC for men in combatting the HIV epidemic,as opposed to the long lag that would occur between infant NTMC and its potential benefit for HIV risk reduction.Another factor may be reports of adverse events by inadequately skilled and over-stretched providers.
In a 2017 report,the CDC recommended routine infant NTMC for HIV prevention in 12 high priority countries[21].Various local bodies fighting the epidemic have also endorsed the procedure[21-26].But presumably Lempertetal[19] had in mind socio-economically advantaged countries such as the UK and North America that have a relatively low HIV prevalence.The negative Canadian Paediatric Society policy nevertheless concluded that in Canada “there may be a benefit [from NTMC] for some boys in high-risk populations and circumstances”[27].
Lempertetal[19] quote the KNMG as saying “it is reasonable to put off circumcision until the age at which [the] boy himself can decide about the intervention or can opt for any available alternatives”.But this disregards the fact that,in early infancy,risk is minimized,and lifetime health benefits are maximized by NTMC.By postponing the procedure until the “boy himself can decide”,the boy is deprived of the early benefits,such as a 10-fold reduction in risk of urinary tract infection(UTI)[28],as well as reduced risk of inflammatory and physical problems during childhood.Since procedural risk is lowest for NTMC performed in early infancy[29],delay also means an increased risk of harm to the boy from an adverse event.Thus,the longer the delay the lower will be the benefit to risk ratio.
The benefits of neonatal NTMC(and % affected based on population prevalence of uncircumcised males and of the medical condition)are:(1)A 90% decreased risk of UTI at age 0-1 years(with 1.3% affected),85% lower risk at 1-16 years(2.7% affected),70% reduced risk at > 16 years(28% affected),as found in a meta-analysis of males of all ages)[28];(2)almost complete elimination of risk of phimosis,with an observational study finding 12% of uncircumcised British males still have phimosis by the age of 18 years[30];(3)a 68% decreased risk of balanitis(10% being affected),as found in a meta-analysis of 8 studies[31];(4)60% decreased risk of candidiasis(thrush;with 10% affected)[31];(5)a 70% decreased risk of HIV infection during heterosexual sex or insertive anal intercourse(with 0.1% affected),as found in a metaanalysis[32];(6)a 53%-65% decreased risk of high-risk human papillomavirus(HPV)infection(4%-10% affected)according to meta-analyses[33-35];(7)a 30% decreased risk of herpes simplex virus type 2 infection(with 4% being affected)based on randomized controlled trial(RCT)findings[36-39];(8)a 50% decreased risk of genital ulcer disease(with approximately 1% affected),based on observational studies[40-42] and a meta-analysis[43];(9)a 40%-55% decreased risk of syphilis infection(with 1% affected)based on the findings of a meta-analysis[43] and observational studies[44,45];(10)a 50% decreased risk ofTrichomonasvaginalisinfection(with 1% affected),according to a RCT[46];(11)a 40% decreased risk ofMycoplasmagenitaliuminfection(with 0.5% affected)as revealed by RCT findings[47];(12)a 50% decreased risk of chancroid(with < 1% affected),according to a meta-analysis[43];(13)a 67%-99% decreased lifetime risk of penile cancer(with 0.11%-0.15% affected),as found in the most recent meta-analysis[4] and observational studies[48-50];and(14)10% decreased risk of prostate cancer(with 1% being affected),as determined by meta-analyses[51-53].
A common cause of inflammatory foreskin conditions such as balanitis can be poor hygiene,medications(such as antibiotics),allergens(including latex condoms,propylene glycol in lubricants),some spermicides,and corticosteroids.Ammonia released from urine by bacterial hydrolysis of urea can cause inflammation of the glans and foreskin.Frequent washing with soaps containing topical allergens or irritants is another common cause of contact dermatitis.Microorganisms are often responsible.
No adverse effect on sexual function or pleasure was found in multiple systematic reviews and meta-analyses[54-58].The most recent found pain during intercourse and erectile dysfunction were significantly lower in circumcised men[57].
A drawback of NTMC includes risk of a minor adverse event,which affects 0.4% in infancy,8% at age 1-10 years,and 4% at ages ≥ 10 years[29].Risk of a major complication is extremely low.Another is cost,which can be substantial if the procedure is not covered by third party insurance.In the UK the National Health Service(NHS)covers medical MC,but not NTMC.If either is performed later,the time taken for the procedure and for the immediate recovery period will mean disruption of daily activities,including employment and school attendance.If the mature male is sexually active,then abstinence from sexual activities will be required during the healing period,which is generally 6 weeks.
PROCEDURAL RISKS MISUNDERSTOOD
The suggestion by Lempertetal[19] that procedural risks are similar “between infants and adults” is not the case.A US study of 1.4 million NTMCs by CDC researchers found risk of adverse events is 10-20 times higher after the neonatal period[29].
At “age 2-18” circumcision is often for treatment of medical problems,usually phimosis,excessive foreskin and lichen sclerosus,which would have been prevented by NTMC in early infancy.Lempertetal[19] ignore many key issues,such as those associated with UTIs that are 10-fold higher in uncircumcised infants.These include the excruciating pain of UTI,the need for blood collection,lumbar puncture,hospitalization for intravenous antibiotic administration,and risk of sepsis,death,and treatment challenges from burgeoning antibiotic resistance[59-62].Early NTMC also means immediate and lifetime abatement of risk of numerous other adverse medical conditions that have varying degrees of morbidity,and,for some,a risk of mortality.Various clinical experts have likened NTMC to a “surgical vaccine”[63,64].In contrast,the overwhelming majority of procedural complications from NTMC in early infancy are minor,and easily and fully resolvable[29].
MEDICAL NEED VERSUS PREVENTION
Lempertetal[19] state that “circumcision is rarely required for medical reasons”,citing studies that reported the need for surgery in 1.7%-2.5% of boys < 18 years[65,66].These figures do not,however,include the much greater number who will develop a foreskin-related problem(mostly phimosis)that infant NTMC would have prevented.Nor do they include infections and diseases that will occur over the lifetime of uncircumcised males with a healthy foreskin.As well,some will require therapeutic circumcision to treat a medical condition at ages > 18 years.The benefits of circumcision when indicated for treatment include treatment of the devastating foreskin inflammatory condition lichen sclerosus,for paraphimosis when emergency intervention must be performed to prevent ischemia and gangrene,as a cure for intractable phimosis that has failed to respond to other interventions such as steroid treatment,and for treatment of cancerous tissue which frequently involves the foreskin of penile cancer patients.
The potential benefits of foreskin retention are its potential use as a skin graft during surgical repair of hypospadias,or to treat burns or other injuries in some specific areas of the body.There may be cultural reasons for retaining the foreskin,in which having the same general genital appearance as other males in non-circumcising cultures may help the boy or man fit in.This was recognized by the AAP in its recommendation that parents “will need to weigh the medical information in the context of their own religious,ethical,and cultural reasons and practices”[16,67].Another is the requirement of a foreskin in the uncommon sexual practice of “docking”[68].
Health authorities have provided advice on care of an uncircumcised penis[69]:Gently,not forcefully,pull the foreskin away from the tip of the penis.Rinse the tip of the penis and the inside part of the foreskin with soap and water.Return the foreskin back over the tip of the penis.
As calculated in risk-benefit analyses for Anglophone countries[70-72],including the United Kingdom[73],approximately half of British males will likely experience a medical condition during their lifetime that NTMC might have protected against.Men can be reluctant to see a medical practitioner when they have a medical problem,especially when it involves their genitalia or sexual dysfunction.
COMPARISON WITH LABIAPLASTY
Lempertetal[19] argue that if “the ‘better in infancy’ view applied with equal force to ‘infant labiaplasty’”,and that “even if the data were unambiguous … the presumable consensus of Western medical ethicists and legal experts would be that such data are irrelevant”[19],citing Reisetal[74].But dataarerelevant,and it is far from clear that the consensus would be otherwise.Evidence-based medicine is held in high regard by professionals for good reason-it works.The ethics(and legality)of a medical procedure must be guided by the best available scientific data,or else incorrect decisions,adverse outcomes and bad laws can result.In the case of labiaplasty the science is clear-it has no significant benefits,so there is no rational justification for performing it on a minor in the absence of a clear medical indication.NTMC,in contrast,does have clear benefits established by a very large body of scientific research data,and the optimal time is early infancy,as supported by the data.NTMC is thus unequivocally evidence based.The reference[74] used by Lempertetal[19] to support their argument is to an opinion piece about surgery on intersex infants.This is a poor analogy as intersex is a complex set of conditions.These may be associated with hormonal imbalances in the womb,or chromosomal abnormalities,and patients have a high risk of later identifying with a gender other than the one decided for them in infancy by a surgeon.
ETHICS
Because NTMC involves surgery on the healthy tissue of a child who is too young to give his consent(consent instead being given by his parents or guardians),and the health benefits during infancy and early childhood are modest(although high over the lifetime),individuals such as Lempertetal[19] argue that childhood NTMC is unethical.Public health ethics attempts to be practical by seeking decisions that will likely produce the greatest net benefit.Well-informed public health authorities might logically be persuaded by the strong evidence favoring NTMC.The extensive reviews by the AAP and CDC led these major authorities to conclude that since the benefits of infant NTMC exceed the risks,parents have a right to choose NTMC for a child.It has been argued that NTMC is justifiable as a public health necessity[75].
The Brussels Collaboration on Genital Integrity(BCGI)[76] decided that an intervention to alter a bodily state should be regarded as a medical necessity when the bodily state poses a threat to the person’s well-being.While absence of NTMC may not pose a “threat” at the time at which NTMC is usually performed,the scientific evidence shows that if not circumcised early in life,approximately half of uncircumcised males will suffer an adverse medical condition over their lifetime because of their uncircumcised state[70-73].Given the degree and breadth of benefits conferred by NTMC,performing infant and childhood NTMC appears consistent with the BCGI’s statement.
Given the wide-ranging protection afforded by NTMC against diverse medical conditions and infections in infancy and childhood,including sexually transmitted infections(STIs)in sexually active adolescent males,it has been argued that it would be unethical not to circumcise boys early in childhood[77,78].Article 24 of the United Nations Convention on the Rights of the Child[79] contains the statement:
“States Parties recognize the right of the child to the enjoyment of the highest attainable standard of health ...States Parties shall strive to ensure that no child is deprived of his or her right of access to such health care services”.
Article 24 states that the definition of health includes preventative health.Thus,not advising parents of benefits and risk of NTMC may violate the rights of the child.Logically,Article 24 might be seen as mandating NTMC,since not circumcising boys poses a threat to their health[78].
Article 5 is also noteworthy.The text reads:“States Parties shall respect the responsibilities,rights and duties of parents or,where applicable,the members of the extended family or community as provided for by local custom,legal guardians or other persons legally responsible for the child,to provide,in a manner consistent with the evolving capacities of the child,appropriate direction and guidance in the exercise by the child of the rights recognized in the present Convention”[79].
Should NTMC be delayed until later,the BMA guidance advises in “card 2,Ten good practice points” that “3.Children who are able to express views about NTMC should be involved in the decision-making process.4.Where a child(with or without competence)refuses NTMC,the BMA cannot envisage a situation in which it will be in a child’s best interests to perform circumcision,irrespective of the parents’ wishes.” Curiously,item 5 states:“It is the parents’ responsibility to explain and justify requests for circumcision,in terms of the individual factors in relation to a particular child’s best interests.” In contrast,the AAP guidance states:“It is important that clinicians routinely inform parents of the health benefits and risks of male newborn circumcision in an unbiased and accurate manner”.
THE “DELAY UNTIL THE MALE CAN DECIDE FOR HIMSELF” ARGUMENT
The policy of deferring early NTMC until an age of consent is reached involves an appeal to “autonomy”.Whilst superficially and emotionally appealing,it is not consistent with evidence and thus appears to be misplaced as we will now explain.The argument fails to consider a more valid concern about beneficence or the best interests of the infant,and a fairer allocation of resources in society.In high-HIV settings,where striving for as high an uptake of NTMC as possible is vital to curb the HIV epidemic,a policy of deferring the procedure would mean fewer circumcisions and hence more infections,increased pressure on health systems,as well as higher health care costs(because later NTMC is more expensive),suffering,social costs and deaths.Even without the risk of HIV infection,deferring infant NTMC would still mean higher incidence of medical conditions that NTMC protects against,and thus higher morbidity,mortality,and costs.We therefore question if that is ethical?
Lempertetal[19] assert that “only a small minority of non-circumcised men report ‘ever’ wishing that they ‘had been’ circumcised—even in the United States,where infant circumcision remains a dominant cultural practice”.As support they cite two articles by their article’s co-author Earp.The first[80] cites a YouGov poll that found 10% of circumcised US men wished they had not been circumcised.But Lempertetal[19] ignore the same poll’s finding that 29% of uncircumcised US men wished they were circumcised.Twenty-nine percent is not a “small” minority,as claimed.Their second citation[81] is to a survey of Amazon Mechanical Turk cohort participants.These were described in their first citation[80].In the latter article,15.9% of uncircumcised men wished they were circumcised,whereas 13.6% of circumcised men wished they were not[81].Thus,slightly more uncircumcised than circumcised men were unsatisfied(1 in 6vs1 in 7).Since both surveys showed higher dissatisfaction amongst uncircumcised men,and the percentages are not small,the references cited by Lempertetal[19] do not support their claim.
Lempertetal[19] reference an article by Earp &Darby that states that “nontherapeutic circumcisions are rarely sought by adults with intact genitals,even in cultures in which circumcision is common and normative”[80].A footnote on page 43 of that article cites a US study of men-who-have-sex-with-men(MSM)that found most were unwilling to have NTMC to prevent HIV.But a single study asking just MSM a hypothetical question is not representative of the majority view.In contrast,a systematic review of over 40 studies across multiple countries and cultures found that when all men are properly informed about NTMC they usually respond positively,and are more positive the better informed they are[82].The VMMC program to combat the African HIV epidemic resulted in circumcision of almost 30 million men by 2020[20],and men continue to queue in some African countries to obtain the procedure.This does not support the critics’ “rarely sought” statement.That many uncircumcised men outside of high-HIV settings(or circumcising cultures)do not wish or seek circumcision may reflect their lack of motive(low HIV risk),lack of free availability,or lack of education about the procedure’s benefits.
Lempertetal[19] go on to argue that men who wish to be circumcised at least have the option of undergoing the procedure,unlike those circumcised as infants,who cannot reverse the decision.Whilst true,this overlooks the barriers to adults seeking the procedure.Lempertetal[19] acknowledge that there will be “certain costs and inconveniences”.But their argument downplays the broad spectrum of barriers(Table 3).

Table 3 The advantages of non-therapeutic male circumcision in neonates compared with older boys and men
CDC researchers conducted a study of adverse procedural events involving 1.4 million medical NTMCs in the US across all ages[29].Amongst the 1.3 million infant NTMCs,adverse event frequency was 0.4%.The CDC referred to these findings in its 2018 policy statement[17].Of the 1400920 reimbursement claims,95.3% were for males aged ≤ 1 year,2.0% were for ages 1-9 years,and 2.7% were for ages ≥ 10 years and above.Compared with infancy,adverse events were 20-times higher in boys aged 1-9 years,and 10-times higher in those aged ≥ 10 years[29].The most common risks were minor bleeding,post-operative clearing of adhesions and removal of excess foreskin[29].Such adverse events are easily and quickly resolved with no lasting effect.An exception is very rare fatal hemorrhage as a result of undiagnosed hemophilia and botched circumcision by poorly trained or negligent operators.In a large California study,frequency of complications was 0.5% in neonates,but in non-neonates was 18.5 times greater[17].A United Kingdom study found complications were 1% amongst boys aged 3-16 years receiving therapeutic MC[83].All were minor and there were no major complications.
A risk-benefit analysis for the United Kingdom[104] found benefits exceeded risks by > 100:1 and estimated that if not circumcised early a large proportion of males would be at risk of an adverse medical condition during their lifetime from a condition attributable to foreskin retention.
In settings where the procedure is freely and readily available,many men who would like to have a circumcision are nevertheless deterred by barriers such as fear of pain,need for sexual abstinence during the healing process,loss of earnings,inconvenience,embarrassment,and various psychosocial factors,as demonstrated by a voluminous literature(see review[84]).In developed countries,a man wanting to be circumcised,but who does not have a medical indication for circumcision,would have to attend a private clinic.In the UK,the cost of an elective adult NTMC is approximately £2259[85],which would be unaffordable to many.In contrast,the cost of an infant NTMC by a private provider is about 10-times lower[86,87].One might wonder whether the “delay until the male is old enough to decide for himself” argument is used by NTMC opponents such as Lempertetal[19] to reduce the likelihood of NTMC ever happening.The multiple advantages of infant NTMC over adult NTMC have been highlighted in multiple reviews[16,17,71-73,88-90](Table 3).
A systematic review of arguments opposing NTMC found that these were supported mostly by low-quality evidence and opinion and were contradicted by strong scientific evidence[18,91].Many of those arguments have been stated above.Others included in the first systematic review[18] were that opponents appear to favor waiting until an adverse medical condition arises and then treating it by methods other than circumcision.However,such methods tend to be only partially effective,require prolonged intervention,and may have side effects.Steroids to treat phimosis is an example.In the meantime,the male will continue to suffer.Circumcision can not only be the definitive choice up front-but will provide at least partial protection against the elevated risk of the array of other adverse medical conditions over the lifetime of the uncircumcised male.Although penile cancer affects only about 0.1% of males over their lifetime[4,90,92],the consequences are devastating.Since childhood NTMC may provide almost complete protection against this cancer,that patient may regret his parents’ failure to have him circumcised.Sexual function and pleasure are often referred to by opponents,likely because problems with these may not be discussed by men affected.A later section is devoted to this issue.
AN ALTERNATIVE TO NTMC FOR JEWISH FAMILIES
Just as is true of the BMA guidance document,Lempertetal[19] see NTMC as mostly a religious practice.They point out the existence of Jewish groups that reject NTMC.Those groups instead practice “Brit Shalom”(Covenant of Peace),a “gender-inclusive welcoming ceremony for children of Jewish parents” who prefer not to have their male children circumcised[93].Brit Shalom arose in recent decades.It provides ritual options for families not affiliated with a synagogue and who may question NTMC.Instead of NTMC,the ceremony may involve cutting a pomegranate instead of a foreskin,and mainly focuses on naming the baby and welcoming him(or her)into the Jewish faith[93].The reasons for replacing Brit Milah with Brit Shalom by some families appear to be respect for gender equality,response to local culture,acceptance of the arguments of NTMC opponents,perception of stigma being associated with circumcision,and Jewish feminism[93].But Lempertetal[19] fail to acknowledge that the practice of Brit Shalom is by a very small minority within Judaism[93].Orthodox Jews reject such alternatives to Brit Milah.The fastest growing section of the Jewish community,at least in Israel,is the Ultra-Orthodox[94] who would never relinquish NTMC on the eighth day of life.In addition,the Reform and Conservative movements,which essentially represent mainstream Judaism,continue their support and practice of Brit Milah.The following is a statement provided to author Mark Sheldon by Rabbi Mark Cooper,Director of the National Organization of American Mohalim(NOAM)and Brit Milah Program of Report Judaism,a program under the auspices of the Hebrew Union College(HUC),Jewish Institute of Religion(JIR):
“Brit Milah,or Jewish ritual or ceremonial circumcision,is widely endorsed in the American Jewish community for Jewish families of various configurations.The Reform Movement of Judaism,under the academic supervision of HUC-JIR in Los Angeles,has sponsored the Brit Milah Program since 1984,with the aim of recruiting,training,and supporting physicians who wish to serve their communities as mohalim.Graduates of the program,currently numbering over 100 physicians and nurse midwives,belong to NOAM.The Conservative Movement of Judaism,under the organizational supervision of the Rabbinical Assembly,likewise sponsors its Brit Kodesh program,with a similar aim.Both movements are committed to perpetuating Brit Milah as Judaism’s oldest continuously practiced ritual and enduring symbol of an unyielding commitment to the continuity of the Jewish way of life”.
Lempertetal’s statement that “Children do not always grow up to share the religious or metaphysical beliefs,nor the associated cultural values,of their parents” is a valid point,and is one reason why infant NTMC can only be rationally justified on scientific,evidence-based grounds[19].
EVIDENCE-BASED VS NON-EVIDENCE BASED
Unlike the BMA’s guidance and European position statements on NTMC of boys,those of the AAP[16,67] and CDC[17,88] are evidence-based and were supported by comprehensive reviews of the best data available at the time.Contrary to these are ones,such as Dutch and Scandinavian,cited by Lempertetal[19],that ignore most of the literature concerning the established benefits of the procedure,and focus instead on issues of ethics,human rights,consent,and legalities,making them essentially ideological positions rather than scientific evidence-based ones.
Lempertetal[19] disparage the AAP’s infant NTMC policy statement,saying it “was met with unprecedented criticism from international experts for falling short of its usual scientific standards and exhibiting strong evidence of cultural bias”[95-98].However,they fail to acknowledge the detailed rebuttals that those claims attracted[15,99-103](Table 2).The “cultural bias” argument by Frisch and his mostly northern European(in particular Scandinavian)co-authors[95] was rebutted by the AAP Task Force on circumcision as applying more logically to northern Europe,where NTMC is rare,than to the US where the proportion of circumcised and uncircumcised males is more equal[15].In response to the AAP,Earp &Darby argued that in Western medicine the bias is “against medically unnecessary surgeries performed on nonconsenting minors”[80].But,unlike the anti-NTMC position,Western medicine might be seen as having a “bias” that is in favor of evidence-based medicine.Two of the most highly rated clinical practice guidelines for NTMC[104]were found by Canadian authors,who could be regarded as non-partisans in the debate,to be the evidence-based policy recommendations by the AAP and CDC.
Lempertetal[19] point out that all AAP policy statements automatically “expire” after 5 years,thus implying that the AAP’s infant NTMC policy is no longer valid.It nevertheless remains the most up-to-date,evidence-based statement by a pediatric body to date.The AAP is,moreover,the world’s largest pediatric body.
QUESTIONABLE ASSERTIONS ABOUT PROTECTION AGAINST HIV
Lempertetal[19] claim that there is no evidence anywhere in the world that NTMC of infants or children reduces the risk of HIV transmission,whether to males or to females.That is not true.Some of the observational studies in Africa that identified the connection between lack of NTMC and risk of HIV were in countries where NTMC of infants and children is the norm[105,106].And studies in Asia and the developed world where NTMC is usually performed in infancy or childhood have found the same[107,108].The evidence favoring childhood NTMC for HIV risk reduction has been reviewed recently[134].
Lempertetal[19] refer to “recent evidence from United Kingdom-comparable epidemiological environments within the Global North,including Canada and Denmark” that show NTMC does not protect against HIV.In support,they cite a Canadian study by Nayanetal[109] that found a non-significant 2% lower HIV prevalence amongst circumcised men.But a detailed analysis of those data by one of the present authors showed that the apparent lack of a significant effect stemmed from the disproportionately high prevalence of HIV infections amongst MSM,the majority of whom adopt the receptive role during anal intercourse,a sexual practice in which being circumcised affords no protection against HIV infection[110,111].Circumcised men in the study who engaged in heterosexual intercourse or who were MSM practicing insertive anal intercourse were at 70% lower risk of HIV infection(P= 7.2 × 10-10)[110,111],just as found in the most recent meta-analysis of all studies globally[112].Nayanetal[113] agreed with those calculations[110].
The same problem of failing to consider MSM in the analyses affected findings in the Danish study cited by Lempertet al[19] of HIV and other STIs amongst men who had undergone NTMC in childhood[114].This was pointed out in a brief critique[115],and in much more detail in a comprehensive critique that also identified multiple other problems with the Danish study[111].
Lempertetal[19] also assert that “there is no evidence of a benefit to female partners of circumcised men,whether in Africa or elsewhere”.This is untrue.Systematic reviews have found that NTMC protects the female partners of circumcised men indirectly by reducing the likelihood that a sexual partner will become infected[116,117].Furthermore,the studies cited by Lempertetal[19] do not support their claim.Two[118,119] were general discussions that predate by up to a decade the data-based studies we cite above.The other[120] was to a trial in which some HIV-infected men ignored advice and resumed sex before their circumcision wounds were fully healed,leading to infection of some female partners,a situation that may not have arisen had they been circumcised in infancy.
SEXUAL FUNCTION AND PLEASURE
Lempertetal[19] criticize the BMA’s guidance for failing to address this topic.In common with assertions by other NTMC opponents,Lempertetal[19] claim that “the foreskin is the most sensitive part of the penis to light-touch sensation both to light touch stimulation and sensations of warmth” and “is a potential source of pleasure in its own right”[19].In support,they cite a weak study[121] critiqued previously[122].That study[121] appeared as a chapter in a 2006 book by NTMC opponents.They also cite a 2007 San Francisco study funded by NOCIRC(an anti-circumcision organization)of sensitivity to light touch[123],but not the critique pointing out flaws in the study’s statistical analyses,methodology and recruitment[124].In contrast,a Canadian study by Bossioetal[125] tested touch,pain,warmth and heat pain,finding that the foreskin is not the most sensitive part of the adult penis across all sensation types examined.Lempertetal[19] ignored the latter study and its findings that tactile sensation of the foreskin was similar to a control point on the forearm,and that there were no differences in sensitivity of other penile sites between circumcised and uncircumcised men.
The “light-touch sensation” Lempertetal[19] focus on involves Meissner’s corpuscles.The histological data confirms the physiological data by showing that the foreskin has no role in sexual sensation or pleasure.Histologically,the neuroreceptors responsible for sexual sensation and thus pleasure have been described as genital corpuscles which are concentrated in the highly innervated coronal ridge of the glans and the underside of the distal shaft of the penis,thus ruling out the foreskin as a histological source of sexual pleasure[126].Meissner’s corpuscles,which are mechanoreceptors,are the most abundant sensory corpuscles in the glabrous skin of the prepuce,and are identical in structure to Meissner’s corpuscles in fingers[127].Whatever the neurological origins of erogenous sensation may be,it is not Meissner’s corpuscles.Thus,the fixation on the light-touch sensation type in publications opposing NTMC is irrelevant.The BMA was right to disregard it in its guidance.
There is abundant high-quality evidence from randomized controlled trials,cohort and case-control studies,and large,well-designed cross-sectional surveys,that medical NTMC has no adverse effect on sexual function,pleasure or satisfaction in men,as summarized in all systematic reviews[54,56,57,128] and meta-analyses[55,57].Significantly,three of these were not by individuals often involved in the NTMC debate and were from non-circumcising countries(Denmark and China,although one author of the Danish study was of Jewish heritage).
Systematic reviews found women,including those from non-circumcising cultures,overwhelmingly prefer a circumcised penis for sexual activity[154,155].Across countries,cultures and sexual preference,a majority of men too regard being circumcised as esthetically pleasing and more sexually desirable to women[129-135].While esthetics is clearcut,sexual pleasure may be purely physical,or could be influenced by psychological factors.Women may have a valid perception of better hygiene and lower risk of STIs if their male partner is circumcised.
Lempertetal[19] quote from a recent review by Tyeetal[136] that speculated about the inability of circumcised men to experience the phenomena of “gliding”,“rocking”,“rolling” or “moving” of the foreskin,and their supposed need for lubrication during sexual intercourse.But they failed to acknowledge that Tye &Sardi’s review stressed that there are no data supporting such phenomena.A recent article examined the claims made by Tye &Sardi and found no evidence that any were of importance[122].When asked which were the most erogenous parts of the penis,men put the glans first,and the foreskin last[137].
INAPPROPRIATE ANALOGIES
Lempertetal[19] wondered why NTMC should be legal whereas “female genital mutilation”(FGM)“is illegal in the United States and most other developed countries”.But this is a false analogy.Most forms of FGM are anatomically dissimilar to MC.FGM confers no medical benefits,only risks.In contrast,NTMC confers a wide range of benefits that greatly exceed risks,especially when performed early in infancy.The two are therefore not comparable,and thus represent separate issues.A FGM case in the United Kingdom,in which the presiding magistrate was Sir James Munby,was misconstrued by NTMC opponents[138].The latter failed to reveal that items 72 and 73 of the judgement recognized substantial health benefits of childhood NTMC that differentiated it from FGM[139].A critical evaluation of the judgement can be found in McAlister[140].
The female equivalent of MC is “hoodectomy”-the removal or reduction of the clitoral hood(female prepuce).It may be done for medical reasons-such as inflammation-the female equivalent of balanitis[141] but can be chosen by women for perceived improvement in sexual function.A number of clinics in the UK offer the procedure.This is not remotely equivalent to the mutilations practised in some North African countries,so to bundle these all together as FGM is unhelpful.
The Lempertetal[19] critique referred to tattooing as being “analogous” to NTMC of minors.But they failed to state whether tattooing confers medical,sexual,or hygienic benefits.For an analogy to be valid,the two must be comparable.Tattooing is not a prophylactic procedure,and we are unaware of it having any proven health benefits.NTMC would appear unique as far as benefits are concerned.Childhood vaccination has some parallels but does not involve removing body parts.Tooth extraction-for example when teeth cause overcrowding of the mouth-comes to mind,but then an overcrowded mouth is a pre-existing problem that can be serious in that it may lead to impacted molars.Various procedures commonly performed on minors and that attract little criticism include cosmetic surgery,such as the removal of birthmarks,or straightening of crooked teeth.But it is curious to us that removal of the foreskin,a well-known haven for bacteria and other microorganisms that play varying degrees of responsibility in the etiology of UTI,HIV,oncogenic HPV genotypes and some other STIs,inflammatory dermatological conditions,physical problems,penile cancer,and prostate cancer in uncircumcised men,and an increased risk of cervical cancer and several STIs in female partners,is a topic of derision by particular minority groups who oppose NTMC of children.
UNTRAINED PRACTITIONERS
Lempertetal[19] raise concerns about NTMC being carried out by untrained practitioners.We share these concerns insofar as the procedure should only be carried out by those who are well-trained and who abide by accepted clinical practice guidelines.This should not preclude a well-trained Jewish mohel,for example,from carrying out the procedure.Research both in developing and developed world settings has shown that,if properly trained and provided with adequate resources,nurses,midwives and physician assistants can perform the procedure to just as high a standard as doctors and surgeons[142-146].Consistent with the studies cited,the BMA guidance states “Male infant circumcision does not require a medical professional”[1].This contradicts Lempertetal[19],who claim the BMA guidance states:“Male infant circumcision does not require medical expertise”.Their misquote is somewhat out of context.The only place in the BMA guidance where the word “expertise” is used is in the preamble,entitled “About this toolkit” on the second page,which states,“We note that there is no requirement in law for these practitioners to have proven expertise,although there are standards that some practitioners ascribe to set by external collectives,associations and societies.” The BMA’s guidance goes on to acknowledge that there have been rare cases of serious injury or death caused by “non-doctor practitioners” and “urge parents who are considering having their child circumcised,to ensure that the practitioner who carries out the circumcision has undergone relevant training and has proven experience and competence in the practice”,a caution the guidance repeats two pages later.
Clearly the BMA was aware of the problem of inadequately trained practitioners causing harm and urge parents to seek trained and experienced providers.We share Lempertetal’s concern that there is no legal requirement in the United Kingdom for a provider to have appropriate training in NTMC,or to abide by particular standards.It is right and proper to draw attention to this issue[19].
LEGAL CONCERNS BY THE CRITICS
In part(1)of their 2ndtable,Lempertetal[19] state that NTMC “has been ruled to amount to ‘significant harm’ within the meaning of the Children Act 1989 by the High Court(Family Division)in the context of care”,and in part(2)that it “has been held,again by the High Court,to amount to greater harm than at least some of WHO Types 1,2,and/or 4 FGM which are agreed to be unethical and unlawful procedures”[19].Each is followed by a footnote(“p”),which discusses the ruling by Lord Justice Munby in 2015[139] in which Lempertetal[19] point out that Munby decided that NTMC constituted “significant harm” on the grounds that it was more invasive than some forms of FGM which were already considered “significant harm” in law.We disagree.Munby set out to decide whether a case of FGM amounted to “significant harm” and agreed that it did.In item 69 Munby states “In my judgment,if FGM Type IV amounts to significant harm,as in my judgment it does,then the same must be so of male circumcision.” Then in item 73,Munby states “there is a very clear distinction between FGM and male circumcision.FGM in any form will suffice to establish ‘threshold’ in accordance with section 31 of the Children Act 1989;male circumcision without more will not.” Lempertet al[19] therefore appear to have misrepresented Munby’s judgement.
Sir William Patrick Dean,a High Court Judge(and former Governor General of Australia),stated in a 1992 case that NTMC,“for perceived hygienic-or even religious-reasons…plainly lies within the authority of parents of an incapable child to authorize surgery on the basis of medical advice"[147].It should be noted that at that time the medical evidence favoring NTMC was not as strong as it is today.
Thus,our evaluation of much of the legal evidence referred to by Lempertetal[19] shows that they have ignored key statements by judges and authoritative organizations that contradict their stance that is opposed to NTMC of boys[19].
As an aside,in relation to FGM,it seems to us difficult to comprehend how the mildest forms of FGM,which may be no more than a prick or scratch,can be construed as “significant harm.” An accidental scratch,cut,or bruise that heals fully within a week or two should not be considered “significant harm”,even though it may damage more skin,cause more pain,and shed more blood than type IV FGM.The definition of “significant harm” is too broad here.There is unarguably a temporary harm in NTMC as the wound heals,but once healed(a process which is much faster in the neonate than the 6-8 weeks required for post-circumcision healing in an adult)there is no harm,as indicated by the multiple studies referred to above showing that sexual function,pleasure,and satisfaction are unimpaired,even improved following the procedure.The “significant harm” assertion was also heavily criticised by a British Law postgraduate[140].Lempertetal[19] ignored this.They also ignored items 72 and 73 of Munby’s judgement which recognized health benefits of boyhood circumcision that distinguish it from FGM.
Lempertetal’s 2ndtable,part(e)[19],states that “Under English criminal law,the imposition of [NTMC] on a nonconsenting adult certainly amounts to the criminal offence of Actual Bodily Harm,and very likely amounts to the offence of Grievous Bodily Harm”[148].But does it? This comment refers the reader to their footnote “s” which states:“See Crown Prosecution Service,Code for Crown Prosecutors,‘Offences against the Person,incorporating the Charging Standard’ [available at cps.gov.uk/Legal-guidance/offences-against-person-incorporating-charging-standard].” Since the word “circumcision” does not appear in that document,the reference fails to support Lempertetal’s argument[19].
The authors go on to suggest that “Either ‘minor’ forms of FGM will have to be allowed,as prominent defenders of child [NTMC] are increasingly proposing ….or [NTMC] of minors will have to be brought into closer alignment with existing standards applied to other practices”.We would,however,question whether the authors of the 9 references they cite are “prominent defenders” of NTMC.If having just a few publications on the topic of NTMC makes one a “prominent” defender of NTMC,one wonders what Lempertetal[19] would make of authors with a prolific publication record,whose findings agree with the medical evidence supporting NTMC.We are,moreover,unaware of any prominent defender of NTMC who also defends any version of FGM.The “prominent defenders” that Lempertetal[19] refer to do not defend FGM on “medical grounds” but recognize the existence of cultural issues.
At the end of their article,Lempertetal[19] provide Notes to their Table 3,where their item marked “l” states:“A subsequent report by the U.S.Centers for Disease Control,apparently produced in coordination with the AAP,was met with similar international criticism[149].For further discussion of the specific problems with these American analyses by one of us see Ref.[151]” Lempertetal[19] ignore the responses to those criticisms[151].They cite a criticism by Kupferschmidetal[149],which was just one of many submissions to the CDC that followed release of the CDC’s draft policy in 2014[17,151].The Kupferschmid web reference is now unobtainable.The CDC reviewed and provided answers addressing virtually all of the various objections in a separate document in 2018[153].Their “by one of us” article cited in Lempertetal’s quote above was by Earp[150](the author for correspondence on the Lempertetalarticle[19]).They do not,however,cite the co-published rebuttal[151] of Earp’s article.
SUMMARY OF THE CRITICISMS BY LEMPERT ET AL.
The basic tenets of Lempertetal’s criticisms of the BMA’s guidance are encapsulated in their statement:“More generally,we find that selective quotes and evidence,where discussed,operate throughout the guidance in the direction of minimizing problems with [NTMC] and downplaying reasons to object to it,while alluding to unproven or intangible(e.g.prophylactic or psychosocial)benefits of the practice.” Lempertetal[19] can be accused of doing the same,but in the opposite direction.Thus,their article appears to be projection.
Many of the issues and contradictions in the BMA guidance identified by Lempertetal[19] stem from the BMA’s statement not being sufficiently evidence-based.Ultimately,NTMC can only be justified rationally on scientific,evidencebased grounds.Religious circumcision may,however,have had a sound practical basis.The reason for Jewish circumcision is lost in the mists of time,although,if we believe Genesis,Abraham was unable to father a child by his wife Sara until he was circumcised.Islamic circumcision is not a command from on high but part of a whole suite of recommendations for practical health and hygiene,which make sense in the scientific era of today.Modern bathing facilities may have improved on some Islamic cleanliness recommendations,but the health and hygiene benefits of circumcision are unchanged.Many children and adults who drift away from their birth religion understand this and continue to favor circumcision.Although,as Lempertetal[19] correctly point out,there is no guarantee that the infant will continue to follow religious traditions when they grow up.Moreover,performing the procedure for religious and cultural reasons may not be accepted by some individuals outside of those traditions and may even be vehemently rejected.
CLAIMS BY OTHER NTMC OPPONENTS IN THE UK
London urologists Matthew Deacon and Gordon Muir recently published a review[155] examining pros and cons of infant NTMC.Although not addressing the BMA’s statement directly,being UK-based,their review is relevant to the BMA’s guidance,so it would be remiss not to mention it here.Several of the present authors examined it and found it was selective with the literature,misleading and contradictory[155].
Deaconetal’s reply[156] was also problematic.Their complaint about self-citing by their critics wasadhominem.Selfciting shows that an author has published copiously on a topic,it says nothing about the quality of their work.Besides,some on the negative side of the NTMC debate also extensively cite their own and each other’s publications[81].Deacon &Muir ignored a systematic review and meta-analysis of all 27 studies of meatal stenosis[157],instead “cherry picking” an outlier study by an anti-NTMC activist,ignoring the strong criticism it attracted[158].They complain that risk-benefit analyses by the present last author and colleagues have not been replicated ….but no one has tried.They dismissed criticism of their claim that NTMC may increase the need for antibiotics as getting “lost in a statistical debate”,but their claim was based on a gross over-estimate of post-procedural infections,and a false assumption that all such infections require antibiotics.They also misunderstood evidence that circumcision protects against HIV during vaginal intercourse by heterosexual men[108,110,111,159,160] and insertive anal intercourse by MSM[110,111,161,162] in developed countries.Deacon &Muir exaggerate perceived pain from NTMC by including “Minimal pain” and “Acceptable pain” responses in a study on parent’s perception of procedural pain from NTMC,arriving at 70.7%,instead of the more realistic 3.7% for “More than acceptable”,or “Much more pain” in their infant child.Finally,they persist in misunderstanding that it is erogenous sensation,not light touch or heat,that matters during sexual intercourse,and that erogenous sensation is concentrated around the glans and distal shaft,not the foreskin[126,136,137].In short,Deaconetal’s reply failed to properly address the original criticisms[155].
An article by Suttonetal[163] argued that general practitioners(GPs)in the United Kingdom were guilty of referring too many uncircumcised males with foreskin problems to their regional pediatric surgery clinic.A critique pointed out that “circumcision as soon as a problem becomes apparent is by far the most cost-effective solution”[164].In a reply to the criticisms,the article’s co-authors Corbettetal[165] cited dated guidelines in 2006 by the British Association of Pediatric Urologists that has a disclaimer that “this statement is not evidence based”[166].Instead,they refuse to circumcise-even 16-year-old boys who are unable to consummate sexual relations-if they regard their phimosis as “physiological”,that is foreskin constriction without evidence of pathology.The tendency to conserve the foreskin ignores the fact that 50% of cases of lichen sclerosus are only discovered after circumcision,when clinical assessment is conducted[167].Those authors then complained that health care providers lack education about foreskin health in children and that many “would welcome further educational resources.” We hope the present article will address this need.Their claim that on average a GP working in the NHS has an annual caseload of “1700 thousand” patients,is a figure three orders of magnitude higher than the likely actual caseload.Corbettetalal[165] ended by promoting their own website[168],which makes the curious claim that “Your penis produces smegma to help keep it lubricated and prevent dryness”.
TAKING AN EVIDENCE-BASED POSITION
As scientists and professionals,we take a strictly evidence-based approach.If infant NTMC is favored by both risk-benefit and cost-benefit analyses,which the present article affirms,then a logical,evidence-based case can be made independently of religious and cultural considerations.As should be apparent from the evidence presented,such a case can be made,and indeed has been made,by several professional bodies,such as the AAP[16,66],the CDC[17,87],and the Circumcision Academy of Australia[71].Opponents of the procedure are welcome to debate these assessments.That is how science proceeds,but to date the contributions to such debates by opponents have been marred by poor science.
Based on high quality scientific evidence,NTMC has minimal or no adverse effect on sexual function,pleasure,or satisfaction[53-57]-if anything,as shown by the most recent meta-analysis,it reduces sexual dysfunction(less pain,less erectile dysfunction,and more favorable intravaginal ejaculatory latency time)[56].This does not by itself justify the procedure,but it does refute one of the main objections by NTMC opponents,namely that NTMC reduces sexual function and pleasure.NTMC also confers a range of medical,health,sexual and practical benefits,and those benefits are maximal and the risks minimal if the procedure is carried out during the neonatal period.If,as the cumulative evidence strongly suggests is the case,neonatal NTMC is favored based on risk-benefit analyses and is cost saving with minimal harm to the recipient,then it is in the male child’s best interests to be provided with the procedure.As a corollary,it would be unethical to deny infant NTMC to parents who want their sons to be circumcised.It also follows that religious or cultural NTMC,provided it is performed to a high clinical standard,is simply doing a medically beneficial procedure for nonmedical reasons,so neutralizing the ethical objections Lempertetal[19] raise against it.
NTMC is a one-off procedure that is most conveniently performed in early infancy using local anesthesia.In early infancy it is simpler,safer,quicker,cheaper,more convenient,cosmesis is optimum,and healing is faster than later circumcision which presents multiple other challenges,as listed in Table 3.The BMA guidance recognizes the need for the procedure to “be in the child’s best interests”.This should prioritize the child’s immediate and long-term health,and its medical benefits to the United Kingdom population as a whole,rather than merely appeasing the religious and cultural requirements of minorities.Medical practitioners,nurses and other health professionals in the United Kingdom have an ethical duty to present clear and unbiased information to parents of boys and to men regarding the diversity of benefits afforded by NTMC,the net level of lifetime protection against these,the low prevalence of procedural risks,that are especially low for neonatal NTMC,and that,unless otherwise indicated,circumcision will be performed using local anesthesia at that age.If the medical practitioner is unable or unwilling to perform the procedure,she or he should direct parents to a medical practitioner who is competent,experienced,and willing.
Given the evidence,infant NTMC might be considered in a similar manner to childhood vaccination.Vaccination is also an early intervention providing considerable benefits,with low risks.Denial of vaccination by medical professionals is unethical.Infant NTMC confers cost-savings to health systems and individuals[169].
A recent evaluation by Canadian researchers of 13 clinical practice guidelines for NTMC in different countries[103] found the best included those by the CDC and the Canadian Urological Association,followed by the AAP.These were chosen because of the thorough reviews of the medical literature each had performed in developing their NTMC policies.The BMA’s guidance was not amongst the 13 chosen.
Alignment of medical thinking in the United Kingdom-that seems to have changed little over the years-with current high-quality scientific evidence and evidence-based policy statements in the US would better inform practitioners,health authorities,policy makers and governments in the United Kingdom.The outcome would likely be improvements in public health,cost coverage by the NHS,as well as long-term cost savings for the NHS and the United Kingdom taxpayer by reducing the case load of infections and diseases that NTMC protects against.
CONCLUSION
The present review finds that extensive criticism of the BMA’s guidance on NTMC by a member of the United Kingdom’s National Secular Society and his co-authors does not stand up to scrutiny.Their opinions are at odds with widely available high-quality scientific evidence and evidence-based policies by major medical bodies such as the CDC and AAP.
FOOTNOTES
Author contributions:Moreton S and Morris BJ conceived the study,Moreton S and Morris BJ prepared the initial draft of the manuscript,Moreton S,Cox G,Sheldon M,Bailis SA,Klausner JD and Morris BJ provided input to successive drafts.All authors have read and approve the final manuscript.
Conflict-of-interest statement:Stephen Moreton is an editor of,and contributor to http://www.circfacts.org,an online facility that provides evidence-based information on male circumcision.Brian J Morris is a member of the Circumcision Academy of Australia,a notfor-profit,government registered,medical society that provides evidence-based information on male circumcision to parents,practitioners and others,as well as contact details of doctors who perform the procedure.Research performed by Brian Morris is supported by U.S.National Institutes of Health Center of Biomedical Research Excellence grant 1P20GM125526-01A1 but was not used for the present publication.None of the authors receive income from their affiliations or work related to circumcision.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BY-NC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United Kingdom
ORCID number:Stephen Moreton 0000-0003-1918-800X;Guy Cox 0000-0002-3719-1109;Mark Sheldon 0000-0003-2256-2365;Stefan A Bailis 0000-0002-4376-5615;Jeffrey D Klausner 0000-0002-6922-7364;Brian J Morris 0000-0003-2468-3566.
Corresponding Author's Membership in Professional Societies:Circumcision Academy of Australia.
S-Editor:Liu JH
L-Editor:A
P-Editor:Zhang XD
 World Journal of Clinical Pediatrics2023年5期
World Journal of Clinical Pediatrics2023年5期
- World Journal of Clinical Pediatrics的其它文章
- Situs inversus totalis in an asymptomatic adolescent-importance of patient education:A case report
- Prediabetes in children and adolescents:An updated review
- Pre-autism:What a paediatrician should know about early diagnosis of autism
- Renal calcification in children with renal tubular acidosis:What a paediatrician should know
- Brain metabolic profile assessed by magnetic resonance spectroscopy in children with Down syndrome:Relation to intelligence quotient
- Clinical factors predicting rotavirus diarrhea in children:A crosssectional study from two hospitals
