Clinical effect of laparoscopic radical resection of colorectal cancer based on propensity score matching
Yang Liu,Xian-Xue Wang,Yu-Lin Li,Wen-Tao He,Hong Li,Hua Chen
Abstract BACKGROUND The incidence of colorectal cancer (CRC) is increasing annually.Laparoscopic radical resection of CRC is a minimally invasive procedure preferred in clinical practice.AIM To investigate the clinical effect of laparoscopic radical resection of CRC on the basis of propensity score matching (PSM).METHODS The clinical data of 100 patients who received inpatient treatment for CRC at Changde Hospital,Xiangya School of Medicine,Central South University (The First People’s Hospital of Changde City) were analyzed retrospectively.The control group included patients who underwent open surgery (n=43),and those who underwent laparoscopic surgery formed the observation group (n=57).The baseline information of both groups was equipoised using 1 × 1 PSM.Differences in the perioperative parameters,inflammatory response,immune function,degree of pain,and physical status between the groups were analyzed.RESULTS Thirty patients from both groups were successfully matched.After PSM,baseline data showed no statistically significant differences between the groups: (1) Perioperative parameters: The observation group had a longer surgery time,less intraoperative blood loss,earlier first ambulation and first anal exhaust times,and shorter gastric tube indwelling time than the control group;(2) Inflammatory response: 24 h after surgery,the levels of interleukin-6 (IL-6),C-reactive protein (CRP),and tumor necrosis factor-α (TNF-α) between groups were higher than preoperatively.IL-6,CRP,and TNF-α levels in the observation group were lower than in the control group;(3) Immune function: At 24 h after surgery,counts of CD4-positive T-lymphocytes (CD4+) and CD4+/CD8-positive T-lymphocytes (CD8+) in both groups were lower than those before surgery,whereas CD8+ was higher than that before surgery.At 24 h after surgery,both CD4+ counts and CD4+/CD8+ in the observation group were higher than those in the control group,whereas CD8+ counts were lower;(4) Degree of pain: The visual analog scale scores in the observation group were lower than those in the control group at 24 and 72 h after surgery;and (5) Physical status: One month after surgery,the Karnofsky performance score in the observation group was higher than that in the control group.CONCLUSION Laparoscopic radical resection of CRC has significant benefits,such as reducing postoperative pain and postoperative inflammatory response,avoiding excessive immune inhibition,and contributing to postoperative recovery.
Key Words: Colorectal cancer;Laparoscopic;Open surgery;Inflammatory reaction;Immune function;Propensity score
lNTRODUCTlON
Colorectal cancer (CRC) is a common cancer of the digestive system with high incidence and mortality[1].There would be approximately 1.93 million new cases of CRC and 940000 deaths worldwide in 2020,representing 10% and 9.4% of global cancer morbidity and mortality,respectively[2].However,early symptoms of CRC remain unclear.Growing tumors can cause abdominal pain,changes in stool characteristics,bloody stools,and other symptoms.At this time,the disease often progresses to the middle and late stages,and its prognosis is poor[3].Currently,the treatment for CRC is largely based on surgery.Early surgical resection,blocking tumor progression,and avoiding post-diffusion metastasis are key to improving the prognosis of patients with CRC.
Traditional open surgery can effectively remove lesions but has the disadvantages of much trauma,slow recovery of postoperative function,and many complications[4].Laparoscopic surgery has recently become increasingly popular.It can achieve complete resection of lesions and promote rapid recovery of patients after surgery,while reducing surgical side injuries[5].However,laparoscopic surgery is complicated,and the anatomy of the colon and rectum increases its difficulty[6].The application of laparoscopic radical resection of CRC remains controversial at the present clinical stage.Therefore,the clinical data of 100 patients with CRC were retrospectively analyzed in this study,and propensity score matching (PSM) was used to balance confounding variables between the observation group and the control group to control confounding bias and reduce the bias[7].The aim of this study was to explore the clinical effects of laparoscopic radical resection for CRC,and to provide a reference for the selection of clinical surgical modalities.
MATERlALS AND METHODS
Patient characteristics
The clinical data of 100 patients who received inpatient treatment for CRC between January 2022 and March 2023 at Changde Hospital,Xiangya School of Medicine,Central South University (The First People’s Hospital of Changde City) were analyzed retrospectively.Inclusion criteria were: (1) First diagnosed as CRC by histopathological examination;(2) Age ≥ 18 years old;(3) Tumor-node-metastasis (TNM) stage of the tumor was I-III;and (4) Received radical surgical resection,open surgery or laparoscopic surgery.Exclusion criteria were as follows: (1) Previous history of abdominal surgery;(2) Perforation,bleeding,acute intestinal obstruction,and other acute surgeries;(3) Combined with other malignant tumors or malignant tumor history;(4) Combined with major organ dysfunction;(5) Pregnant and lactating women;and (6) Missing the data required for this study.
Operative method
Open surgery: Lithotomy position after general anesthesia.The size and position of the incision was confirmed based on the size and position of the lesion.First,a normal abdominal examination was performed to determine the location of the tumor and its proximal tissues and organs.The upper and lower regular and corresponding mesenteric vessels of the tumor were first ligated,and the intestinal canal was freed.The tumor was removed and intestinal tubes at each end of the tumor and its corresponding mesentery were fitted.Lymph node dissection,intestinal anastomosis,abdominal cavity irrigation,lining drainage,and abdominal cavity closure were completed.
Laparoscopic surgery: Lithotomy position after general anesthesia.Laparoscopic access was established by opening 3–5 small holes (5–10 mm) in the abdominal wall and introducing the laparoscopic and surgical instruments.A 5 cm incision was made in the abdominal wall,based on the location of the lesion,to remove the tumor tissue.A CO2pneumothorax was established,and the intraperitoneal condition was investigated.The mesenteric arterial and peripheral connective tissues were isolated.The tumor,appropriate intestinal tubes at each end of the tumor,and corresponding mesentery were removed,and the lymph nodes were dissected.Colorectal anastomosis was performed,bowel ducts were rationalized,the abdominal cavity was irrigated,internal drainage was performed,instruments were withdrawn,and the abdominal cavity was closed.
Data collection
Data were collected from patients through the hospital information system,including baseline data such as age,sex,body mass index (BMI),tumor diameter,lesion location,and the American Society of Anesthesiologists (ASA) grade.
(1) Perioperative parameters such as surgery duration,intraoperative blood loss,number of lymph node dissections,first ambulation time,bowel sound recovery time,first anal exhaust time,gastric tube indwelling time,and complication rate were compared between the groups;(2) Inflammatory response: Five milliliters of venous blood was collected after fasting preoperatively and 24 h postoperatively.After centrifugation,the levels of interleukin-6 (IL-6),C-reactive protein (CRP),and tumor necrosis factor-α (TNF-α) were determined using an enzyme-linked immunosorbent assay;(3) Immune function: Blood samples were collected as described above.CD4-positive T-lymphocytes (CD4+) and CD8-positive Tlymphocytes (CD8+) counts were quantified using a flow cytometer and companion kit (BD FACSCalibur;Becton,Dickinson And Company.,United States);(4) Degree of pain: The visual analog scale (VAS) was used to evaluate the degree of pain preoperatively and 24 h and 72 h postoperatively.The VAS score is 0–10,with a higher score indicating more intense pain;and (5) Physical status: The Karnofsky performance score (KPS) was used to evaluate the physical status preoperatively,and 1 month and 3 mo postoperatively.The KPS can be divided into 11 grades from disease-free (100 points) to death (0 points),with higher scores indicating better conditions.
Statistical analysis
R software (R 4.1.3;Bell Laboratories.,Auckland,New Zealand) was used for the PSM.The nearest neighbor matching method and the caliper matching method were used.When the caliper value was set to 0.2,age,tumor diameter,lesion location,and ASA were matched at a ratio of 1 × 1 between groups,and the standardized mean difference (SMD) was applied to evaluate the matching effect.SMD < 0.1 can was considered as a good matching effect.SPSS software (version 26.0;IBM Corp.,Armonk,NY,United States) was used for data processing and analysis.Quantitative data according to the Gaussian distribution was described as mean ± standard (mean ± SD),the paired samplet-test was applied to compare within groups and the independent samplet-test to compare among groups.Quantitative continuous data that did not conform to the Gaussian distribution are shown as median (M) and interquartile range [M (P25-P75)],and the Mann–Whitney U test was applied for comparison.Categorical data were expressed as numbers and percentages,n(%),and the chi-square test was applied for comparison.Statistical significance was set atP< 0.05.
RESULTS
Patient baseline data
Among the 100 patients in the study,43 who underwent open surgery were included in the control group,and 57 who underwent laparoscopic surgery were included in the observation group.There were statistically significant differences in age,tumor diameter,lesion location,and ASA between the groups (Table 1).

Table 1 Patients’ baseline data
Patient baseline data after PSM
Sixty patients were successfully matched after 1:1 PSM.The SMD for age,tumor diameter,lesion location,and ASA classification were 0.014,0.090,0.092,and 0.035,respectively,which can be considered a good matching effect.After PSM,there were no significant differences between the groups in terms of age,sex,BMI,underlying disease,tumor diameter,TNM stage,histological type,lesion location,or ASA classification (Table 2).
Comparison of the perioperative parameters
There were no significant differences between the groups in the number of lymph node dissections,bowel sound recovery time,or rate of complications (P> 0.05).The observation group had a longer surgery time,lesser intraoperative blood loss,earlier first ambulation time,shorter first anal exhaust time,and shorter gastric tube indwelling time than thecontrol group (Table 3).
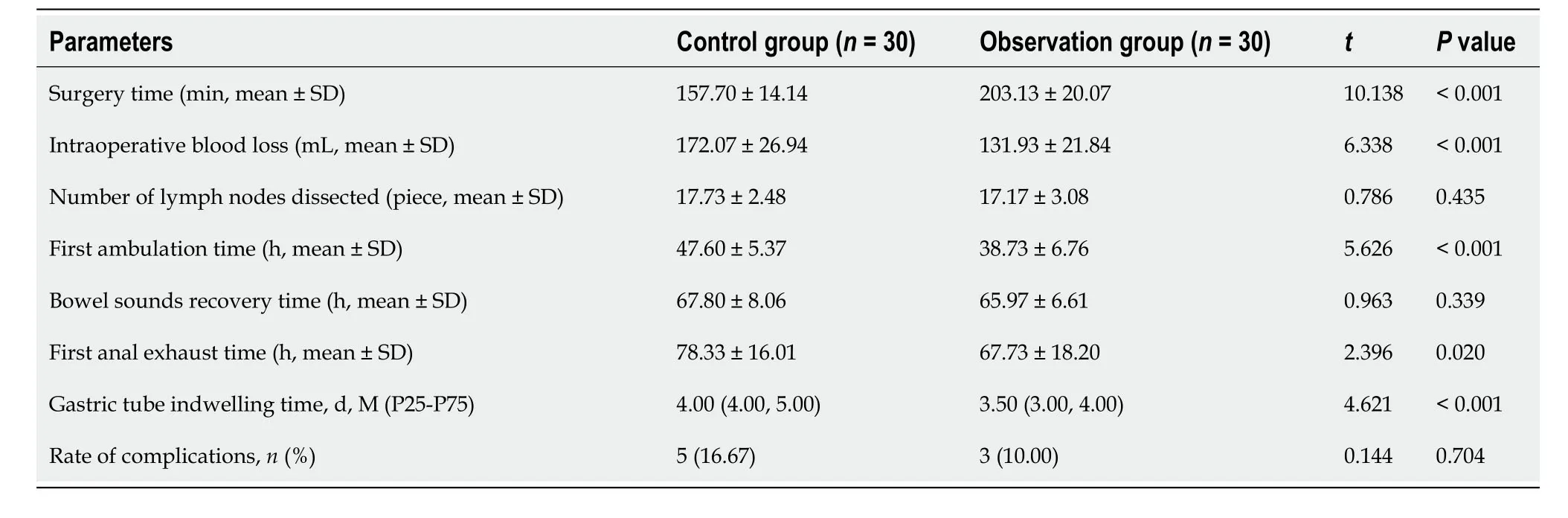
Table 3 Comparison of perioperative parameters between the two groups
Comparison of the postoperative inflammatory indexes
There were no differences between groups in the levels of IL-6,CRP,and TNF-α preoperatively (P> 0.05).At 24 h after surgery,the IL-6,CRP,and TNF-α levels of both groups were higher than preoperatively,and those in the observation group were lower than the control group (Table 4).

Table 4 Comparison of postoperative inflammatory indexes between the two groups
Comparison of the postoperative immune indexes
CD4+counts and CD4+/CD8+in both groups were lower postoperatively and CD8+counts were higher 24 h after surgery.The observation group had higher CD4+counts and CD4+/CD8+and lower CD8+counts than the control group at 24 h after surgery (Table 5).
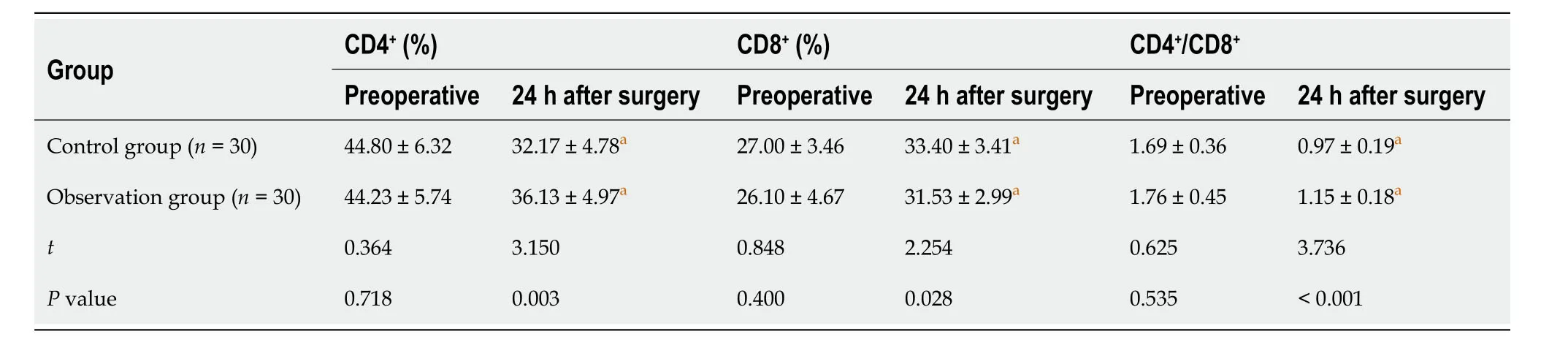
Table 5 Comparison of postoperative immune indexes between the two groups
Comparison of the postoperative VAS scores
Before surgery,the average VAS score of the control group was (3.90 ± 0.55) and the observation group was (3.40 ± 1.67),with no significant differences between groups (P> 0.05).At 24 h after surgery,the average VAS score of the control group was (5.07 ± 1.44) and the observation group was (4.13 ± 0.73).At 72 h after surgery,the average VAS score of the control group was (3.93 ± 0.45) and the observation group was (3.20 ± 0.85).The VAS scores in the observation group were significantly lower than those in the control group at 24 h and 72 h after surgery (Figure 1).

Figure 1 Comparison of the visual analogue scale scores between the two groups. VAS: Visual analogue scale.aP < 0.05
Comparison of the postoperative KPS
Before surgery,the average KPS of the control group was (60.67 ± 12.30) and the observation group was (62.00 ± 9.61).The average KPS of the control group was (65.00 ± 6.82) and the observation group was (69.67 ± 7.18) one month after surgery.The average KPS of the control group and the observation group was (69.00 ± 8.45) and (70.67 ± 6.915) respectively,three months after surgery.Preoperatively and three months after surgery,there were no significant differences in KPS scores among the groups (P> 0.05).The observation group had a higher KPS score than the control group one month after surgery (Figure 2).

Figure 2 Comparison of the Karnofsky performance score between the two groups.KPS: Karnofsky performance score.aP < 0.05
DlSCUSSlON
The etiology of CRC is complex and is linked to diet,digestive tract diseases,lifestyle,genetics,and other factors.The long-term interaction of these factors affects the intestinal peristaltic ability and increases the contact time between carcinogens and the intestine,thus continuously stimulating the intestinal mucosal cells,causing them to proliferate out of control and eventually form tumor tissues[6].With an improvement in living conditions,changes in dietary structure and mode of life have caused a significant increase in the morbidity of CRC,and the age of onset has gradually become lesser[8].Currently,CRC is generally treated based on the principle of clearing the tumor and lymph nodes,and inhibiting the transfer and invasion of cancer cells[9].
Surgery is the only curative treatment for CRC[10].Open radical resection for CRC has a long history of clinical application.An abdominal opening can be used to observe the abdominal cavity and locate the intestinal segment of the lesion,and resection of the tumor and the affected intestinal segment can be completed under direct vision to achieve complete removal of the tumor[11].However,open surgery,with its long incisions and extensive lymph node dissection,is prone to a strong stress response.In addition,the risk of infection increases with a long exposure time of the abdominal cavity,which affects the recovery of the body after surgery[12].Recently,laparoscopic surgery has become increasingly popular for treating CRC.The magnification of laparoscopic images broadens the surgical domain and helps surgeons more clearly identify important structures,such as blood vessels,nerves,and ureters,facilitating delicate surgical manipulation.Laparoscopic surgery results in a smaller wound,which avoids prolonged exposure of the abdominal cavity to air and reduces the damage to the body caused by invasive surgery to a certain extent[13,14].However,laparoscopy has not been completely developed and laparoscopic surgery is difficult[15].Most current studies comparing the efficacy of open surgery and laparoscopic surgery for CRC are retrospective analyses,and confounding factors are generally unevenly distributed,thus affecting the reliability of the conclusions.In 1983,Rosenbaum and Rubin[16].proposed PSM,a subject matching method to reduce confounding effects and balance the difference between the observation group and the control group.This could achieve a balance among the confounding factors through a post-randomization process,thus minimizing the bias in the estimation of the treatment effects[17,18].
We collected clinical data of 43 patients who underwent open radical resection and compared them with those of 57 patients who underwent laparoscopic radical resection for CRC.After 1:1 PSM,60 patients were matched successfully.By comparing perioperative parameters,we found that open radical resection and laparoscopic radical resection for CRC had similar clinical effects,including the number of lymph nodes removed,bowel sound recovery time,and incidence of complications.Laparoscopic radical resection of CRC results in a longer surgery time,less intraoperative blood loss,earlier time to get out of bed and first anal exit,and shorter time to remove the stomach tube.Considering that the visual field of laparoscopic surgery has a planar structure,the surgeon needs to use an instrument to sense the location of the lesion,which enhances the difficulty of the procedure to a certain extent,thus prolonging the surgery time.VAS scores 24 and 72 h postoperatively were significantly lower in patients who underwent laparoscopic radical response for CRC,and they also had a higher KPS one month after surgery.At three months after surgery,there were no significant differences in the KPS scores between the groups.These results confirmed that laparoscopic surgery can reduce early postoperative pain and contribute to early physical recovery.
Invasive surgery can easily induce a stress response,mainly manifested as excessive expression of inflammatory factors[19].On the one hand,the production of large amounts of inflammatory cells can increase the incidence of postoperative infection;on the other hand,it can directly affect the surgical outcome[20].IL-6 and TNF-α are typical proinflammatory factors,which are important mediators that trigger and initiate inflammatory responses.CRP levels can be markedly elevated post-trauma.The results of our study showed that patients receiving laparoscopic radical resection of CRC had lower levels of IL-6,CRP,and TNF-α at 24 h after surgery.This indicates that laparoscopic surgery may reduce the early postoperative inflammatory response compared to open surgery.This is consistent with the results reported by Chenet al[10].At the same time,surgical trauma can also cause the temporary inhibition of immune function[21].CD4+T cells are helper cells and induce T cells with anti-tumor effects,CD8+T cells are inhibitory T cells that inhibit the immune reaction,and CD4+/CD8+is an important marker reflecting the body's immune regulation efficacy[22].The results of our study showed that patients who underwent laparoscopic radical resection for CRC had higher CD4+counts and CD4+/CD8+ratios and lower CD8+counts than patients who underwent open surgery.This suggests that laparoscopic surgery can avoid excessive immunosuppression compared with open surgery.Strong postoperative inflammatory responses and immunosuppression can lead to delayed healing,which is detrimental to the postoperative recovery.
Although PSM was used to eliminate the influence of some confounding factors and increase the reliability of the study results,there are still some limitations: (1) This study has a retrospective design with a low level of evidence;(2) The number of cases included in the study was small,and the research data were all from the same institution;(3) Based on a single-center retrospective study,in addition to demographic and pathological characteristics,there are still some confounding factors regarding the treatment differences,such as chemoradiotherapy regimen and tumor metastasis;and (4) Lack of long-term observation data.Future studies with large sample sizes and high-quality randomized controlled trials are still needed to confirm this.
CONCLUSlON
Our results indicated that laparoscopic radical resection of CRC has significant benefits such as reducing postoperative pain and postoperative inflammatory response,avoiding excessive immune inhibition,and contributing to postoperative recovery.
ARTlCLE HlGHLlGHTS
Research background
Currently,there is some debate about the merits of laparoscopic surgery of colorectal cancer (CRC).
Research motivation
The advantages of laparoscopic surgery for CRC require further validation through additional studies and data.
Research objectives
Exploring the advantages of laparoscopic radical resectionvsopen surgery for CRC.
Research methods
Data from 43 patients with CRC who underwent open surgery and 53 who underwent laparoscopic surgery were compared retrospectively,and differences between the groups were analyzed using 1:1 propensity score matching equilibrium treatment.
Research results
Compared with open surgery,laparoscopic radical resection of CRC showed better early inflammatory,immune,and pain indicators,and better physical status one month after surgery.
Research conclusions
Laparoscopic radical resection of CRC can reduce postoperative pain and postoperative inflammatory responses,prevent excessive immune inhibition,and contribute to postoperative recovery.
Research perspectives
To analyze the early clinical effects of laparoscopic radical resection for CRC.
FOOTNOTES
Author contributions:Liu Y designed and performed the research and wrote the paper;Chen H designed the research and supervised the report;Wang XX and Li H designed the research and organized the data;Li YL and He WT designed the research and contributed to the analysis.All authors approved the manuscript.
Supported byScientific Research Project of Hunan Provincial Health Commission,No.202204114103.
lnstitutional review board statement:The study was reviewed and approved by the Changde Hospital,Xiangya School of Medicine,Central South University (The First People’s Hospital of Changde City) Institutional Review Board,Approval No.2021-265-02.
lnformed consent statement:All patients have signed informed consent forms.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:The clinical data used in this study can be obtained from the corresponding author upon request at 229chenhua@sina.com.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yang Liu 0009-0005-8321-573X;Xian-Xue Wang 0000-0001-7793-7791;Yu-Lin Li 0009-0007-9587-370X;Wen-Tao He 0009-0009-0574-9487;Hong Li 0009-0000-0038-2422;Hua Chen 0009-0006-0423-2847.
S-Editor:Li L
L-Editor:A
P-Editor:Li L
 World Journal of Gastrointestinal Surgery2024年1期
World Journal of Gastrointestinal Surgery2024年1期
- World Journal of Gastrointestinal Surgery的其它文章
- Prospects in the application of ultrasensitive chromosomal aneuploidy detection in precancerous lesions of gastric cancer
- Prognostic value of ultrasound in early arterial complications post liver transplant
- Added value of ratio of cross diameters of the appendix in ultrasound diagnosis of acute appendicitis
- Single-incision laparoscopic transabdominal preperitoneal repair in the treatment of adult female patients with inguinal hernia
- Predictive value of machine learning models for lymph node metastasis in gastric cancer: A two-center study
- Micro-power negative pressure wound technique reduces risk of incision infection following loop ileostomy closure
