Predictive value of NLR,Fib4,and APRl in the occurrence of liver failure after hepatectomy in patients with hepatocellular carcinoma
Tian-Zuo Kuang,Meng Xiao,Yong-Fan Liu
Abstract BACKGROUND Neutrophil-lymphocyte ratio (NLR),fibrosis index based on four factors (Fib4),aspartate aminotransferase-to-platelet ratio index (APRI) can be used for prognostic evaluation of hepatocellular carcinoma.However,no study has established an individualized prediction model for the prognosis of hepatocellular carcinoma based on these factors.AIM To screen the factors that affect the prognosis of hepatocellular carcinoma and establish a nomogram model that predicts postoperative liver failure after hepatic resection in patients with hepatocellular carcinoma.METHODS In total,220 patients with hepatocellular carcinoma treated in our hospital from January 2022 to January 2023 were selected.They were divided into 154 participants in the modeling cohort,and 66 in the validation cohort.Comparative analysis of the changes in NLR,Fib4,and APRI levels in 154 patients with hepatocellular carcinoma before liver resection and at 3 mo,6 mo,and 12 mo postoperatively was conducted.Binary logistic regression to analyze the influencing factors on the occurrence of liver failure in hepatocellular carcinoma patients,roadmap prediction modeling,and validation,patient work characteristic curves (ROCs) to evaluate the predictive efficacy of the model,calibration curves to assess the consistency,and decision curve analysis (DCA) to evaluate the model’s validity were also conducted.RESULTS Binary logistic regression showed that Child-Pugh grading,Surgical site,NLR,Fib4,and APRI were all risk factors for liver failure after hepatic resection in patients with hepatocellular carcinoma.The modeling cohort built a column-line graph model,and the area under the ROC curve was 0.986 [95% confidence interval (CI): 0.963-1.000].The patients in the validation cohort utilized the column-line graph to predict the probability of survival in the validation cohort and plotted the ROC curve with an area under the curve of the model of 0.692 (95%CI: 0.548-0.837).The deviation of the actual outcome curves from the calibration curves of the column-line plots generated by the modeling and validation cohorts was small,and the DCA confirmed the validity.CONCLUSION NLR,Fib4,and APRI independently influence posthepatectomy liver failure in patients with hepatocellular carcinoma.The column-line graph prediction model exhibited strong prognostic capability,with substantial concordance between predicted and actual events.
Key Words: Hepatocellular carcinoma;Hepatic resection;Liver failure;Influencing factors;Columnar graphs
lNTRODUCTlON
Hepatocellular carcinoma is a common malignant tumor,and its incidence and mortality rates are increasing worldwide[1].Hepatic resection is a primary treatment for hepatocellular carcinoma;however,postoperative liver failure is a serious complication that severely affects patient survival and quality of life[2,3].Therefore,an accurate assessment of the risk of developing postoperative liver failure is essential to guide clinical treatment and improve patient prognosis.In recent years,inflammation and fibrosis indices have received extensive attention for prognostic assessment of patients with hepatocellular carcinoma.Neutrophil-lymphocyte ratio (NLR) is the ratio of neutrophils to lymphocytes in the blood and is usually associated with inflammatory responses,infections,tumors,and other diseases[4].The fibrosis index based on four factors (Fib4) is used to assess the degree of liver fibrosis and is often used to evaluate patients with chronic liver disease;the higher the value,the more severe the degree of liver fibrosis[5].The aspartate aminotransferase-to-platelet ratio index (APRI) is the ratio of aspartate transaminase (AST) to platelets (PLT) in the blood,and changes in this ratio can offer insights into the liver’s state and extent of inflammation[6].These three indices are commonly used indicators of inflammation and fibrosis and have been shown to be strongly associated with the prognosis of patients with hepatocellular carcinoma.However,few studies have investigated the predictive value of these indicators in the development of postoperative liver failure and their changes.Therefore,this study aimed to investigate the changes in the levels of NLR,Fib4,and APRI in patients with hepatocellular carcinoma after hepatic resection and to establish a corresponding prediction model to assess their predictive ability in the occurrence of postoperative liver failure.It aimed to provide clinicians with a more accurate prognostic assessment tool,enhancing the prevention and therapeutic outcomes of postoperative liver failure while improving the survival rate and quality of life of patients.
MATERlALS AND METHODS
Objects of study
A total of 220 patients with hepatocellular carcinoma who received treatment in our hospital from January 2022 to January 2023 were selected as the study objects,and were divided into a modeling cohort of 154 patients and a model validation cohort of 66 patients according to a ratio of 7:3.The model validation cohort was divided into liver failure group (n=21) and non-liver failure group (n=45).The study has been approved by the hospital ethics committee.
Inclusion criteria: (1) Meeting the diagnostic criteria for hepatocellular carcinoma[7];(2) the age is above 18 years old;(3) the condition is stable and non-life threatening;(4) all patients received hepatectomy;and (5) complete clinical data.
Exclusion criteria: (1) There are other types of liver cancer;(2) complicated with heart,kidney,lung and other important organ dysfunction;(3) there is a mental system disease;(4) combined with malignant tumor;and (5) not all follow-up work was completed.
Methodology
Observation of grouping and prognosis:At the same time,according to whether the patients had liver failure after hepatectomy,the modeling group was divided into liver failure group (n=53) and no liver failure group (n=101).The validation cohort was divided into liver failure group (n=21) and non-liver failure group (n=45).The outcome was observed,and postoperative liver failure was taken as the end event.Criteria for hepatic failure: Increased international normalized ratios and associated hyperbilirubinemia on or after the 5thd after surgery.
Index observation and method:General data of patients with and without liver failure were collected through electronic medical records of our hospital: Age,gender,body mass index (BMI),smoking history,drinking history,hepatitis B,tumor diameter,cirrhosis,tumor number,Child-Pugh grade of liver function,surgical site,alpha-fetoprotein,and postoperative NLR,Fib4,APRI levels of the two groups were compared to analyze the influencing factors of liver failure in patients with hepatocellular carcinoma after hepatectomy.Build a roadmap prediction model and verify it.
Child-Pugh grading: including the assessment of general condition,ascites,bilirubin,albumin,prothrombin time,etc.,with 1-3 points scored and a total of 15 points,of which 5-6 points are graded as grade A,indicating the presence of a small surgical risk;7-9 points are graded as grade B,indicating the presence of a moderate surgical risk;and ≥ 10 points are graded as grade C,indicating the presence of a large surgical risk.
To analyze the changes of NLR,Fib4 and APRI levels in patients with hepatocellular carcinoma after hepatectomy,as well as their predictive value for the occurrence of postoperative liver failure,and to establish and validate a roadmap prediction model.The formula for calculating NLR: NLR=Neutrophil count/lymphocyte count;the formula for calculating Fib4:APRI calculation formula: APRI=(AST/upper limit normal)/PLT count × 100%.
Statistical analysis
SPSS 26.0 software and R software were used to analyze the data collected in this collection,and all the collected measures were tested for normality by the Shapiro-Wilk method,withP> 0.05 for normally distributed data expressed as (mean ± SD) andt-test,and withP< 0.05 for non-normally distributed data described as median (quartiles) and Mann-WhitneyUtest.Collected count data were expressed as (%),χ2or Fisher exact test was used for data that were unordered,and Mann-WhitneyUtest was used for data that were ordered.Univariate and multivariate logistic regression was used to analyze the factors affecting the development of liver failure after hepatectomy in patients with hepatocellular carcinoma,to develop a predictive model for the column-line diagram,and the discriminative power of the validation set and the calibration plot were used to assess the accuracy of the column-line diagram.The area under the patient operating characteristic curve (ROC) (AUC) was used to evaluate the discriminative ability of the column-line diagram.Calibration curves for the model were calculated and the consistency of the model was verified with the Hosmer-Lemeshaw test.Decision curve analysis was also performed to evaluate the discriminative ability of the model.P< 0.05 was considered a statistically significant difference.
RESULTS
Baseline clinical features
A total of 220 patients with hepatocellular carcinoma were included,including 154 in the modeling cohort and 66 in the model validation cohort.The mean age of the patients was (53.11 ± 2.58) years,with 124 males (56.36%) and 96 females (43.64%).There were 86 males (55.84%) and 68 females (44.16%) in the modeling cohort.There were 38 males (57.58%) and 28 females (42.42%) in the validation cohort.The baseline data of the modeling cohort and the validation cohort were shown in Table 1.Except for differences in Child-Pugh grade,surgical site and Fib4,there were no statistically significant differences in other general data between the two groups (P> 0.05,Table 1).

Table 1 Baseline data for modeling queues and validation queues,n (%) or mean ± SD
Comparison of clinical data between the modeling cohort with liver failure and the group without liver failure
There were no significant differences in gender,age,BMI,tumor diameter,resection range and tumor number in the modeling cohort (allP> 0.05).There were significant differences in Child-Pugh grade,surgical site,NLR,Fib4 and APRI between the two groups,and the levels of NLR,Fib4,and APRI indexes in the liver failure group were significantly higher than those in the non-liver failure group (allP< 0.05,Table 2).

Table 2 Comparison of clinical data between the modeling cohort with liver failure and the group without liver failure,n (%) or mean ± SD
Logistic regression analysis of risk factors for liver failure after hepatectomy in patients with hepatocellular carcinoma
Binary logistic regression analysis with liver failure=1 and no liver failure=0 as dependent variables and factors with significant differences in the above univariate analyses as covariates showed that Child-Pugh classification,BCLC stage,NLR,Fib4,and APRI were all risk factors for the development of liver failure after hepatic resection in patients with hepatocellular carcinoma.
The logarithm of the odds of liver failure was modeled using the following equation: Log (P)=2.023 × Child-Pugh grading+1.269 × surgical site+0.505 × NLR+0.569 × Fib4+5.254 × APRI -16.266 (Table 3).

Table 3 Logistic regression analysis of risk factors for liver failure after hepatectomy in patients with hepatocellular carcinoma
Establishment of a nomogram model for predicting liver failure in patients with hepatocellular carcinoma after hepatectomy
Five independent risk factors (Child-Pugh grade,surgical site,NLR,Fib4,and APRI) were obtained by R software to build a prediction model,and a nomogram model was established (Figure 1).After calibration of the generated nomogram (Figure 2A),the predicted event had a high consistency with the actual event.The area under the ROC curve of the nomogram prediction model was 0.692 (95%CI: 0.548-0.830) (Figure 2B).The decision analysis curve is shown in Figure 2C,where the X-axis represents the threshold probability,the Y-axis represents the net return,and the solid black line represents the net return of the prediction model using the nomogram.The curve shows a high return rate,which further confirms the effectiveness of the nomogram prediction model.
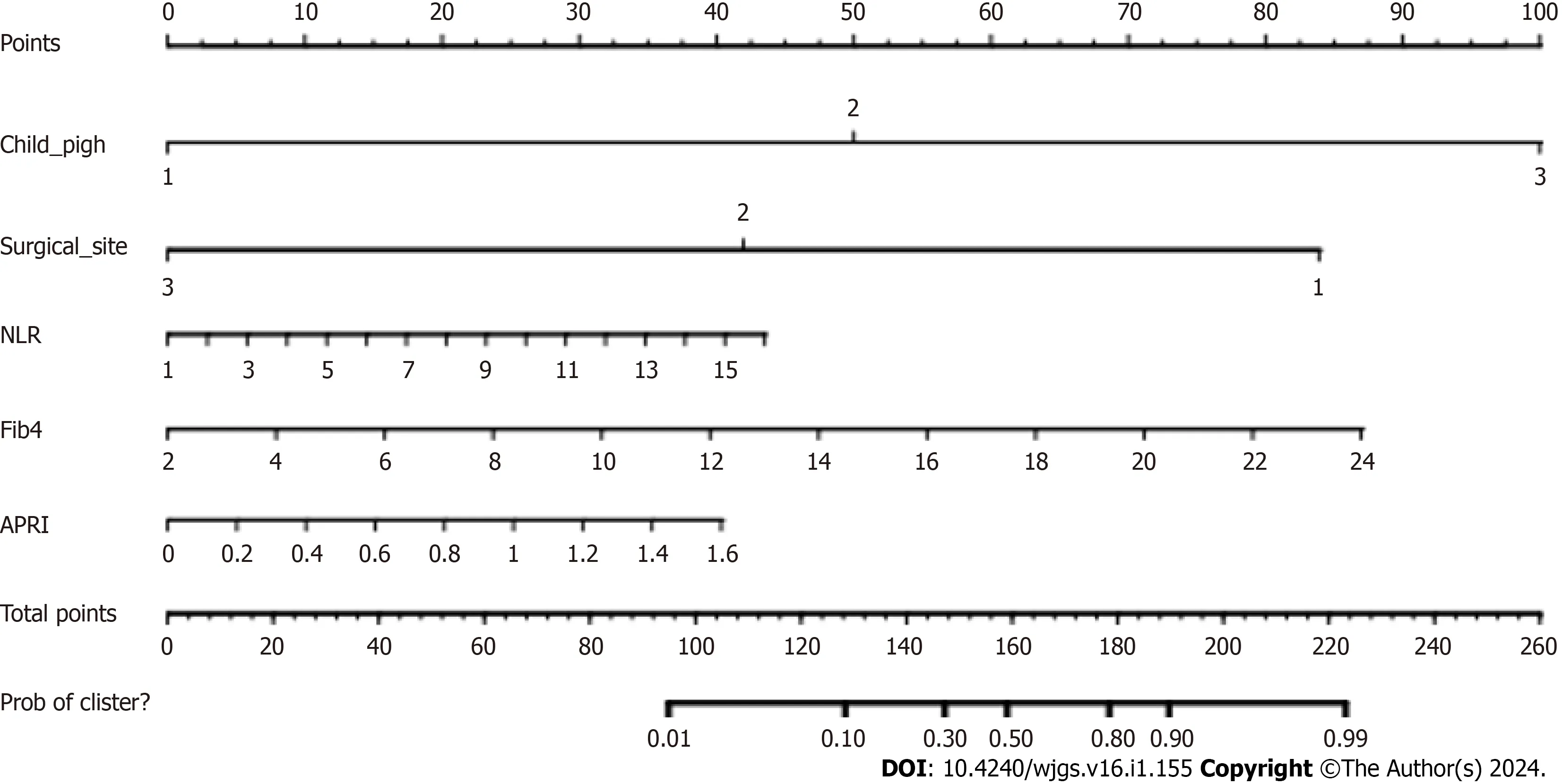
Figure 1 Column line diagram.
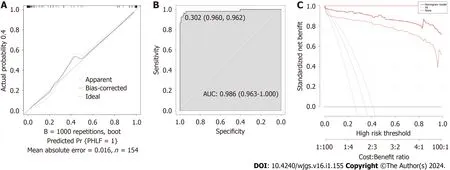
Figure 2 Modeling queue.A:Modeling queue calibration curves;B: Modeling queue patient work characteristic curve;C: Modeling queue decision analysis curve.
Verification of the nomogram model
Based on the clinical data of patients in the validation cohort (n=66) (Table 4),the ROC curve was used for externalvalidation of the ATC risk nomogram,and the results showed that the lower product of the ROC curve was 0.692 (95%CI: 0.548-0.837) (Figure 3A).The slope of the calibration curve of the generated nomogram was close to 1 (Figure 3B),and the result of Hosmer-Lemeshow test wasχ2=1.784,P=0.987.The decision curve shows that the model has a higher net benefit (Figure 3C),suggesting that the nomogram model has better calibration ability in the validation group.

Figure 3 Verification queue.A:Verification queue patient work characteristic curves curve;B: Verification queue calibration curve;C: Verification queue decision analysis curve.

Table 4 Comparison of clinical data between the validation cohort with liver failure and the cohort without liver failure,n (%) or mean ± SD
DlSCUSSlON
In recent years,the safety of hepatic resection has been greatly improved and the perioperative morbidity and mortality rates have been reduced by about 15% with the continuous development of surgical techniques,the widespread use of relevant instruments,and the continuous advancement of intensive care techniques[8].Liver failure after hepatic resection is a progressive multi-organ failure that occurs in about 10% of patients undergoing major liver surgery and includes mild hepatic impairment (characterized by transient hyperbilirubinemia) and severe hepatic impairment (resulting in multi-systemic insufficiency requiring invasive treatment in the intensive care unit)[9].As liver function declines,patients experience persistent hyperbilirubinemia and coagulation disorders,which seriously affect their postoperativeprognosis.Based on this,this study focuses on analyzing the factors influencing the occurrence of liver failure after hepatic resection in patients with hepatocellular carcinoma and establishing a column-line graph prediction model.
In this study,patients were divided into modeling cohort and validation cohort,and clinical data of patients were compared.In the modeling cohort,53 patients (21.90%) with liver failure and 101 patients (78.10%) without liver failure were found,indicating that the prognosis of patients after comprehensive hepatectomy was better.At the same time,by comparing the clinical data of the two groups of subjects in the modeling cohort,it was found that there were significant differences in Child-Pugh grade,surgical site,NLR,Fib4,and APRI between the two groups.Among them,the levels of NLR,Fib4,and APRI indexes in the liver failure group were significantly higher than those in the non-liver failure group,while there were no significant differences in other indexes.Binary logistic regression analysis with liver failure=1 and no liver failure=0 as dependent variables and the factors with significant differences in the above univariate analyses as covariates showed that Child-Pugh grading,BCLC staging,NLR,Fib4,and APRI were risk factors for liver failure after hepatic resection in patients with hepatocellular carcinoma.Child-Pugh grading was mainly based on the following five indicators to assess liver function: Total bilirubin level,serum albumin level,prothrombin time,and the presence or absence of ascites and encephalopathy.Higher Child-Pugh grades (B and C) mean poorer liver function and more damage to liver cells,which can result in the liver not being able to perform its functions properly,including synthesizing proteins,detoxifying and metabolizing medications,making the liver unable to efficiently deal with toxins and wastes produced by the body and increasing the risk of liver failure[10].At the same time,hepatectomy can result in partial removal or damage to the liver,which can affect the function of the liver.The liver has a very important physiological function in the human body,including metabolism,detoxification,synthesis of important proteins,etc.,so even partial resection may have a certain impact on the body.In addition,after hepatectomy,the remaining liver tissue needs to undertake more functions to maintain normal physiological activities,and if the surgical site is removed too far,the remaining liver tissue may not be able to meet the needs of the body,resulting in an increased risk of liver dysfunctionand even liver failure[11].Neutrophil count reflects the pro-inflammatory state of the body and lymphocyte count reflects the immune state of the body,NLR is the ratio of these two values,a high NLR value implies an increased inflammatory response and immune dysfunction which further promotes liver injury,thus greatly increasing the risk of liver failure after surgery[12].In addition,patients with liver failure have a dysregulated immune system,which is characterized by systemic inflammation and immune paralysis,leading to bacterial infections[13].As a result,neutrophils and lymphocytes in the blood of patients with liver failure are generally at a high level,which proves that a high level of NLR is closely related to the development of liver failure,and can be used as a predictive indicator for the development of liver failure.The results suggest that high levels of NLR are closely related to the development of liver failure,and may be used as a predictive indicator of liver failure.
Recently,there has been increasing evidence of the utility of non-invasive liver fibrosis-related markers,such as the Fib4 index[14] with APRI[15].A study observed the value of Fib4 in the prognosis of patients with hepatic failure,and it was noted in the study that patients with hepatic failure tend to have underlying chronic liver disease and cirrhosis,and that Fib4 can,to a certain extent,reflect the level of liver fibrosis in them[16].Fib4 is an important indicator for noninvasive and objective evaluation of liver fibrosis and cirrhosis,and its role in liver fibrosis and cirrhosis is even greater,and the degree of fibrosis is positively correlated with the Fib4 value[17].The same result was also obtained in the study by Zhanget al[18] and is similar to the results of the study in this paper.In addition,APRI also affects the occurrence of postoperative liver failure in hepatocellular carcinoma patients undergoing hepatic resection to some extent.Yugawaet al[19] showed that APRI was the best independent predictor of liver failure after severe hepatic resection in patients with hepatocellular carcinoma,which was similar to the findings of the present study.Although the Child-Pugh score has long been the most commonly used tool for evaluating liver function in the clinic,the Child-Pugh score relies mainly on the observation and judgment of the patient’s symptoms and signs,resulting in possible subjective differences,and can only provide a general risk assessment and cannot accurately predict the occurrence of liver failure.There is a significant correlation between APRI and the degree of fibrosis and hepatic impairment in hepatic histopathology.Among the APRIs,the PLT count is an important factor representing hepatic fibrosis,and a low PLT level has been associated with advanced hepatic fibrosis and liver cirrhosis[20].In addition,serum AST has a high sensitivity to reflect the presence of liver fibrosis or cirrhosis.Therefore,APRI is more accurate in predicting liver failure after hepatectomy.
In order to clarify the predictive value of NLR,Fib4,and APRI in the occurrence of liver failure after hepatic resection in patients with hepatocellular carcinoma,the present study used the modeling cohort to establish a column-line diagram model,the area under the ROC curve of the column-line diagram prediction model was larger,and the predictive efficacy was better,and the subjects in the validation cohort predicted the probability of the occurrence of liver failure in the validation group by the column-line diagram of,suggesting that has a certain predictive value.In addition,the factors of the model are all patients’ medical record data,which are easier to obtain and have higher clinical adaptability.In addition,as can be seen from the validation cohort calibration curve graph,the deviation between the actual outcome curve and the calibration curve is small,indicating that the consistency between the predicted events and the actual events is high.As can be seen from the validation cohort decision analysis curve,the decision analysis curve is located in the upper right corner usually indicates that the model has a high true positive rate and a low false positive rate,which means that this model has a certain degree of accuracy and reliability.
CONCLUSlON
In summary,NLR,Fib4,and APRI are all independent influences on the occurrence of liver failure after hepatectomy in patients with hepatocellular carcinoma.The column-line graph prediction model constructed in this study for the occurrence of liver failure after hepatectomy in patients with hepatocellular carcinoma showed good predictive ability,and the consistency between the predicted events and the actual events was high.The model has a broad potential as a tool to prevent the occurrence of liver failure after hepatectomy in patients with hepatocellular carcinoma.As this study is a retrospective analysis with limited clinical data of subjects,the selection of indicators may not be comprehensive enough.At the same time,there are initial differences in the modeling and verification of groups of patients,which may lead to differences in research results.Therefore,a large sample size and multi-indicator analysis can be conducted in the future to establish a more comprehensive prediction model.
ARTlCLE HlGHLlGHTS
Research background
Hepatectomy is a common surgical procedure for hepatocellular carcinoma,but liver failure can occur after surgery,which is a serious complication that can be life-threatening to some extent.Therefore,predicting the occurrence of liver failure is very important for postoperative management and patient care.Neutrophil-lymphocyte ratio (NLR),fibrosis index based on four factors (Fib4),aspartate aminotransferase-to-platelet ratio index (APRI) are indicators derived from a simple blood test that reflect liver function and degree of fibrosis.By analyzing the relationship between these indicators and the occurrence of liver failure,we can evaluate their potential value in predicting liver failure and provide a basis for clinical practice.
Research motivation
Hepatectomy is an important treatment for hepatocellular carcinoma,but the occurrence of postoperative liver failure may bring serious complications and risks to patients.Abnormal expressions of NLR,Fib4,and APRI are common in patients with liver failure.However,there are few studies on the predictive value and changes of these indicators in the occurrence of postoperative liver failure.
Research objectives
To analyze the expression differences of NLR,Fib4,and APRI in hepatocellular carcinoma patients with liver failure after hepatectomy and their predictive value in postoperative liver failure,and establish and verify their nomogram prediction models.
Research methods
A total of 220 patients with hepatocellular carcinoma who received treatment in our hospital from January 2022 to January 2023 were retrospectively selected as research objects,and were divided into a modeling cohort of 154 patients and a model validation cohort of 66 patients according to a ratio of 7:3.At the same time,according to whether the patients developed liver failure after hepatectomy,The model group was divided into liver failure group (n=53 cases) and no liver failure group (n=101 cases).The model validation cohort was divided into a group with liver failure (n=21 cases) and a group without liver failure (n=45 cases).By comparing the general data of patients,binary logistic regression analysis was conducted to analyze the factors affecting the occurrence of liver failure in patients with hepatocellular carcinoma after hepatectomy,the road map prediction model was established and verified,the predictive efficacy of the model was evaluated by patient operating characteristic curve (ROC),the consistency of predicted events with actual events was evaluated by calibration curve,and the effectiveness of the model was evaluated by decision curve analysis.
Research results
Child-Pugh grade,surgical site,NLR,Fib4,and APRI were all risk factors for liver failure in patients with hepatocellular carcinoma after hepatectomy.In addition,in this study,the deviation between the actual result curve and the calibration curve of the nomogram generated by the modeling queue and the verification queue is small,and the consistency between the predicted event and the actual event is high.The validity of the nomogram prediction model is further confirmed in the decision analysis curve of modeling queue and verifying queue prediction model.
Research conclusions
NLR,Fib4,and APRI were all independent factors influencing the occurrence of liver failure in hepatocellular carcinoma patients after hepatectomy,and the further constructed nomogram prediction model of liver failure in hepatocellular carcinoma patients after hepatectomy showed good prediction ability,with high consistency between predicted events and actual events.This model has broad potential as a tool to prevent liver failure in patients with hepatocellular carcinoma after hepatectomy.
Research perspectives
This study is a retrospective analysis with limited clinical data of subjects,and the selection of indicators may not be comprehensive enough.At the same time,there are initial differences in the modeling and validation of groups of patients,which may lead to differences in study results.Therefore,more clinical indicators need to be added for further comprehensive evaluation and a more comprehensive prediction model needs to be established.
FOOTNOTES
Author contributions:Kuang TZ contributed to investigation,software,data curation,formal analysis,and writing-original draft;Xiao M contributed to methodology,supervision,and validation;Liu YF contributed to conceptualization,resources,writing-review,and editing.
lnstitutional review board statement:The study was reviewed and approved by the Medical Ethics Committee of Ji’an Central People’s Hospital.Institutional Review Board (Approval No.2021-L121201).
lnformed consent statement:All study participants,or their legal guardian,provided informed written consent prior to study enrollment.
Conflict-of-interest statement:The authors have no conflicts of interest to declare.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yong-Fan Liu 0000-0002-1740-6950.
S-Editor:Chen YL
L-Editor:A
P-Editor:Xu ZH
 World Journal of Gastrointestinal Surgery2024年1期
World Journal of Gastrointestinal Surgery2024年1期
- World Journal of Gastrointestinal Surgery的其它文章
- Prospects in the application of ultrasensitive chromosomal aneuploidy detection in precancerous lesions of gastric cancer
- Prognostic value of ultrasound in early arterial complications post liver transplant
- Added value of ratio of cross diameters of the appendix in ultrasound diagnosis of acute appendicitis
- Single-incision laparoscopic transabdominal preperitoneal repair in the treatment of adult female patients with inguinal hernia
- Predictive value of machine learning models for lymph node metastasis in gastric cancer: A two-center study
- Micro-power negative pressure wound technique reduces risk of incision infection following loop ileostomy closure
