Stromal lenticule addition keratoplasty with corneal crosslinking for corneal ectasia secondary to FS-LASlK:a case series
Li-Xiang Wang, Ying-Ping Deng, Meng-Zhen Xie,2, Ke Ma, Hong-Bo Yin, Qiong Wang,Rui Gong, Jing Tang
1Department of Ophthalmology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
2West China School of Medicine, Sichuan University, Chengdu 610041, Sichuan Province, China
Abstract
● KEYWORDS: corneal ectasia; femtosecond laserassisted in situ keratomileusis; stromal lenticule addition keratoplasty; corneal crosslinking; corneal thickness;corneal biomechanics
INTRODUCTION
With the increased myopia rate and greater acceptance of surgical correction, corneal refractive surgery has experienced booming growth in the recent decade.Femtosecond laser-assistedin situkeratomileusis (FS-LASIK)is currently a popular way of corneal refractive surgery that is suitable for different grades of myopia[1].The creation of a corneal flap and the associated large cut greatly change the normal corneal biomechanical property and secondary corneal ectasia is found in 90 per 100 000 eyes receiving LASIK surgery, which is 4.5 times higher than that in photorefractive keratometry (PRK) and 8.5 times in small incision lenticule extraction (SMILE)[2-3].Currently, corneal crosslinking is a first-line therapy for keratoconus and corneal ectasia that improves the biomechanical strength of the cornea and can reduce the risk of further ectasia[4-5].However, patients with extremely thin cornea are contraindicated from conventional corneal crosslinking due to the toxicity of riboflavin dye to the corneal endothelium and intraocular tissues[6].The application of corneal transplantation on these advanced staged patients isalso limited by the shortage of donor cornea grafts and the risk of rejection associated with immune intolerance[7-8].Here we report a case series of 5 patients who received the addition of a lenticule collected from myopic SMILE patients under the original corneal flap, which provides a promising therapy to cope with this condition.
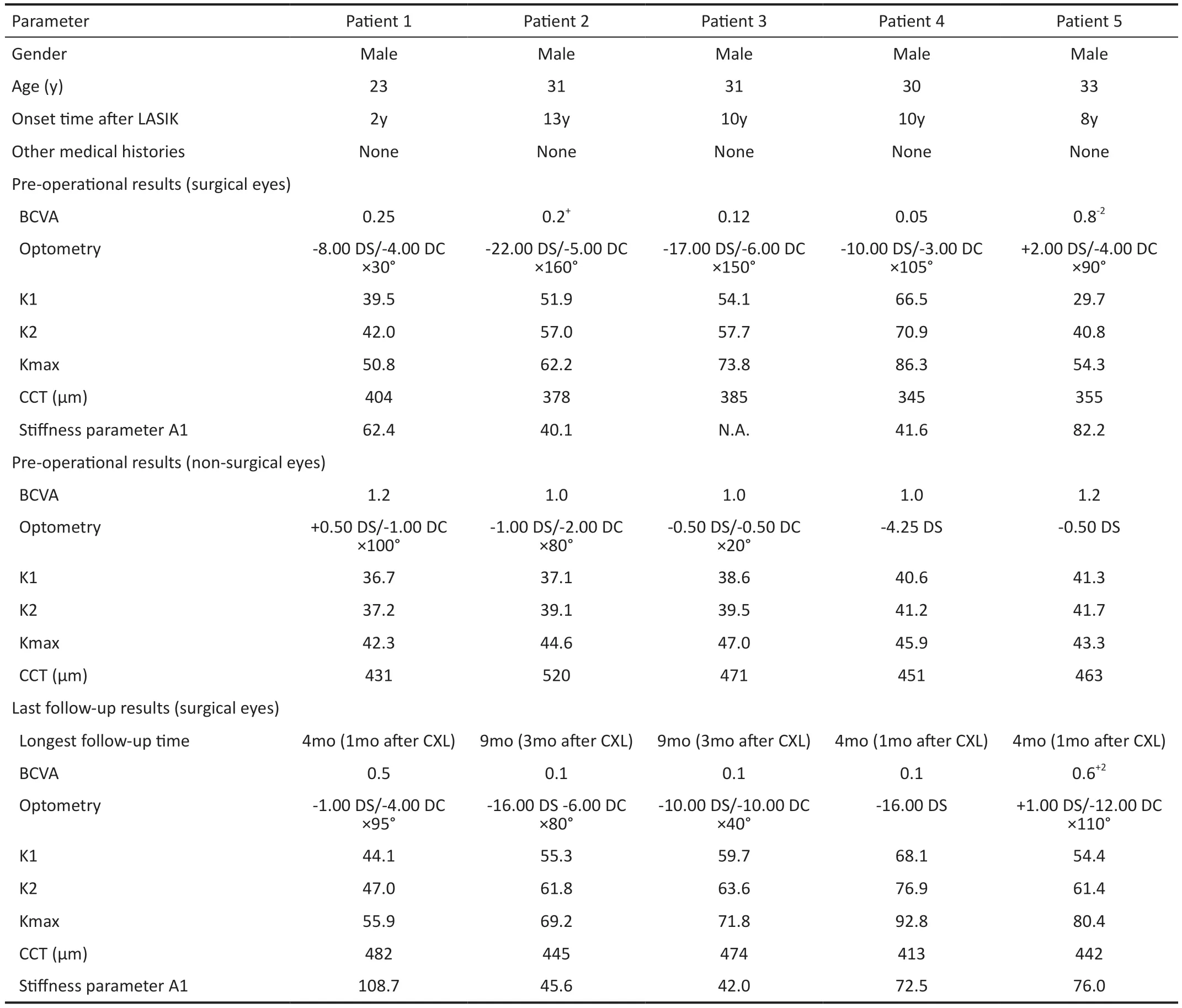
Table 1 Pre-operational demographic information and post-operational follow-up results
SUBJECTS AND METHODS
Ethical Approval The study was approved by the Ethics Committee of West China Hospital of Sichuan University(approval number 2023552) and was performed in accordance with the declaration of Helsinki.Informed consent was obtained from all subject.
A total of 5 male patients who developed corneal ectasia secondary to FS-LASIK received stromal lenticule addition keratoplasty (SLAK) and corneal crosslinking between September 2021 and December 2022 in West China Hospital.Their ages ranged from 23 to 33y, and the onset time from FS-LASIK surgery ranged from 2 to 13y.All patients denied a history of other eye disorders, eye trauma, and other eye surgeries than FS-LASIK.The detailed pre-operational demographic information and primary examination results of the surgical eyes are summarized in Table 1.SLAK and corneal crosslinking were suggested as the most suitable surgical method due to their thin cornea and the disease’s progressive nature, with written informed content and the agreement to use figures and data for publishing acquired before surgery.
All surgeries were conducted by the same surgeon under topical anesthesia following the standard protocol.SLAK and corneal crosslinking were conducted as 2 separate surgeries, with a time gap between 3 to 6mo.Briefly, in SLAK, the corneal flap was first gently lifted with a spatula, and a stromal lenticule with a suitable thickness collected from a seronegative donorwho received small incision lenticule extraction (SMILE) for the correction of myopia was placed in position.The thickness of the lenticule was determined by the thinnest total corneal thickness before surgery, and the expected thickness at the thinnest point after intrastromal lenticule addition keratoplasty should be at least 450 μm to enable the safe application of corneal crosslinking.The refractive power of the lenticule was not deliberately selected, and the remaining refractive error of the patient was supposed to be corrected by a rigid gas-permeable lens or scleral lens after the refractive power stabilized.Then the corneal flap was placed back with its margin carefully matched with the stromal bed.Patients received topical anti-inflammatory eye drops, artificial tears,and antibiotics for 1mo after the surgery.Corneal crosslinking was conducted after complete relief of corneal edema.Patients received either deepithelized or transepithelized mode, with the same ultraviolet A (UVA) exposure diameter as 9 mm.The selection of deepithelized or transepithelized crosslinking was based on the flap thickness and willingness of the patient, and patients with a thin flap of less than 100 μm were advised to select the transepithelized mode as the extremely thin flap after deepithelization may lead to an increased surgical challenge to prevent flap dislocation and associated higher risk of epithelial ingrowth.The detailed surgical parameters are demonstrated in Table 2.After the surgery, patients were given bandage lenses, topical antibiotics, and fluorometholone eye drops.All patients were followed as scheduled, and best corrected visual acuity (BCVA), optometry, non-contact tonometer (Oculus,Germany), Corvis ST (Oculus, Germany), Pentacam (Oculus,Germany), anterior segment optical coherence tomography(AS-OCT, Tomey, Japan) were prescribed as needed.

Table 2 Surgical parameters of stromal lenticule addition keratoplasty with corneal crosslinking
RESULTS
All surgeries were successfully conducted with no significant complications.Patients generally showed stabilized keratometry and corneal topography after the combination therapy.Figure 1 demonstrate the trend of keratometry and total corneal thickness changes after the 2 consecutive surgeries, and detailed followed-up eye examination results are summarized in Table 1.Transient corneal edema was observed right after SLAK, which gradually resolved within 3mo.The addition of a lenticule under the corneal flap resulted in a substantial gain of total corneal thickness between 50-90 μm in the 5 patients after complete relief of corneal edema.In addition, a change of corneal topography and refractive status was also evident, and a further increase of corneal keratometry of the anterior surface due to the elevation of the cornea after lenticule addition was noted in all patients, especially in the early stage after SLAK.Two patients had improved BCVA(patient 1 from 0.25 to 0.5 and patient 4 from 0.05 to 0.1).However, 3 patients showed decreased BCVA (patient 2 from 0.2+to 0.1, patient 3 from 0.12 to 0.1, and patient 5 from 0.8-2to 0.6+2) due to irregular astigmatism and transient haze formation after crosslinking.Four patients showed an increase in the corneal biomechanical property after the combination therapy, as reflected by increased stiffness parameter A1 in the Corvis ST.A demonstration of corneal changes following the two procedures is shown in Figure 2.The photography of the surgical eyes of all patients at their latest follow-up visit was demonstrated in Figure 3.
DISCUSSION
In this case series, we report for the first time the effect of combination therapy of SLAK plus corneal crosslinking for the treatment of corneal ectasia secondary to FS-LASIK.The implanted lenticule showed good biocompatibility with its adjacent tissue and the keratometry and corneal thickness became stabilized after 3mo.Our data support the primary efficacy and safety of this new technique in the short term,which has the potential to become a promising therapy for LASIK-associated secondary ectasia in the future.

Figure 1 Trend of keratometry and corneal thickness change after the combination therapy and the intrastromal haze early after corneal crosslinking Change of keratometry and total corneal thickness at the thinnest point of patients 1 to 5 from baseline to the latest follow-up visit after the combination therapy.CXL: Corneal crosslinking.

Figure 2 Anterior segment OCT and corneal topography of patient 4 at different time points A: Before surgery; B: 1mo after stromal lenticule addition keratoplasty, showing mild corneal edema; C: 1mo after corneal crosslinking.
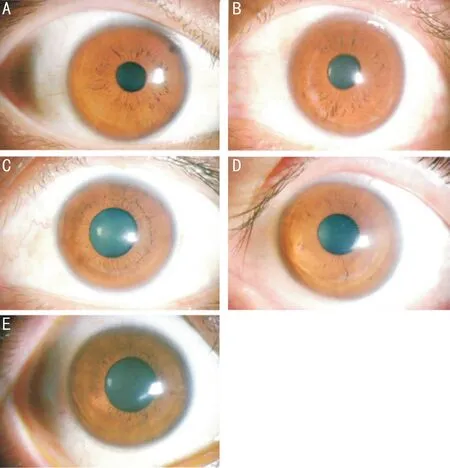
Figure 3 Photography of the surgical eyes at the latest follow-up visit A-E corresponds to patients 1 to 5, respectively.
Stromal lenticule implantation keratoplasty has become an emerging technique for keratoconus and secondary ectasia that shows superior safety and tolerability compared to conventional keratoplasty surgeries, including penetrating keratoplasty and deep anterior lamellar keratoplasty[9-10].Patients receiving stromal lenticule implantation keratoplasty have a faster recovery and needn’t rely on long-term immunosuppression therapy to prevent graft rejection[11].In some previous reports, the implanted lenticules were fabricated from cadaver donor corneas with a laser, and the size, refractive power, and thickness were specifically designed that matched the recipient data.Most of these lenticules are designed to be negative meniscus in shape, which compensates for the central steepening topography of corneal ectasia and keratoconus[12-14].For patients with asymmetric corneal ectasia, the lenticule can be further fabricated into specialized forms, such as dog-nut,ring, or crescent shapes that balance the protrusion at different sites[15-16].However, this technique is greatly limited by the severe shortage of donor cornea[7].Thus, currently, lenticules collected from SMILE surgery have now become a major source of stromal lenticule implantation keratoplasty, which can be readily collected in refractive centers as a “surgical waste” that has been discarded for a long time in the past[17].Lenticules collected from myopic SMILE patients are positive meniscus in shape, which generally has a central thickness between 70-170 μm, a peripheral thickness between 10-30 μm, and an optic zone diameter between 5.0-7.0 mm depending on the surgical design[18].Conversely, hyperopic SMILE surgery is now becoming an emerging technique,which provides negative meniscus lenticules that have a thinner center, but it is not conducted as a conventional surgery for hyperopia in most refractive centers[19-20].In our case series,lenticules collected from myopic SMILE were chosen due to their better availability, the thinner peripheral edge for better flap repositioning, and greater central thickness that enables subsequent corneal crosslinking and provides a substantial gain of central corneal thickness.As demonstrated by the examination data during follow-ups, the patients showed an increase of corneal thickness by 50-90 μm as expected, which was consistent with the thickness of the implanted lenticule and generally remained stable after 3mo.However, the addition of lenticules from myopic SMILE surgery resulted in a further elevation and increase of keratometry in our patients,which also stabilized after 3mo.The increased elevation is expected, as the positive meniscus-shaped lenticule adds more thickness to the center.The implantation of lenticule substantially changed the topography of the recipient’s eye, but the change of refraction can be poorly predicted before surgery and astigmatism remained irregular.Thus, patients still need further refractive correction after the surgery, such as rigid gaspermeable lenses or scleral lenses after their refraction status stabilized[21-22].
The addition of a lenticule under the flap enables the safe application of corneal crosslinking to further enhance its biomechanical property and reduce the risk of ectasia.Corneal crosslinking has become a first-line therapy for patients with keratoconus and corneal ectasia that builds up covalent crosslinks between stromal lamella with riboflavin under UVA exposure and sound evidence supports its role in strengthening the corneal architecture[23].However, due to the cytotoxicity of UVA to the corneal endothelium and intraocular tissues,corneal crosslinking can only be safely conducted when the total corneal thickness exceeds 400 μm[6].In our case series, all patients were contraindicated for crosslinking at first due to their extremely thin cornea, but the addition of a lenticule under the flap enables the conduction of the surgery.Corneal crosslinking was conducted 3-6mo after SLAK as transient edema compromised the accuracy of measurement.The demarcation lines were observed in all patients in the deep stroma under the lenticule.The combination therapy resulted in a general improvement in corneal biomechanical strength, as reflected by the substantial increase of stiffness parameter A1 in the Corvis ST test in 4 patients.Two methods of crosslinking, including the deepithelized mode and transepithelized mode were explored.Previous studies found that the deepithelized mode resulted in a higher presence of the demarcation line and better control of keratometry due to the better penetration of riboflavin into corneal stromal, but the transepithelized mode showed advantages of better BCVA and greater corneal thickness[24].
In our study, no adverse events or serious complications were reported in these 5 cases.However, SLAK under an existing corneal flap theoretically shared common risks with FS-LASIK surgery, which includes flap-related complications, epithelium ingrowth, and lenticule dislocation[16,25].In recent years, an alternative surgical method to implant the lenticule within a corneal stromal pocket created by femtosecond laser for the treatment of keratoconus has been explored[11-12,14,16,26-29].Compared with our cases, they may show potential advantages of reducing the risk of lenticule dislocation as it is more firmly implanted[26].However, as the remaining stromal bed is thin in patients with advanced corneal ectasia, creating a new stromal bed may elicit further risk of disease progression and the implantation process has been reported to cause complications such as perforation and laceration that eventually leads to surgical failure[11,29-30].Thus, in our study, we choose to use the existing flap to allocate the lenticule instead of creating a new stromal pocket.
As far as we know, this is the first case series demonstrating the surgical outcomes of the combined application of SLAK and corneal crosslinking for the treatment of corneal ectasia secondary to FS-LASIK surgery.The two surgeries are conducted with no need for the creation of a new cut, as the corneal flap created during FS-LASIK provides a natural opening to insert and hold the lenticule.Our study and the technique have some limitations.First of all, the follow-up time is short and the long-term efficacy of the combination therapy to prevent corneal ectasia can’t be determined.Second,as a pilot study of the new technique in our refractive center,although 2 different methods including the deepithelized and transepithelized modes are explored, the study lacks sufficient sample size and statistical power to draw a conclusion on the selection of crosslinking method.Third, the selection of the parameters of the implanted lenticule is primarily judged by the surgeon’s experience.However, as demonstrated by the study results, the post-operational refraction and corneal topography can be poorly predicted and how to choose a more appropriate lenticule needs exploration.In addition, irregular astigmatism is a major reason for the decreased vision of the patient and a further decrease of BCVA in 3 patients indicates the need to focus on ways to improve vision in future research.In conclusion, our case series reports the feasibility, efficacy,and safety of applying SLAK and corneal crosslinking for patients who developed corneal ectasia after FS-LASIK.The combination therapy is suitable for patients with extremely thin cornea that are contraindicated for corneal crosslinking and can become an alternative selection besides corneal transplantation for these patients.
ACKNOWLEDGEMENTS
Foundations:Supported by the Science & Technology Department of Sichuan Province (China) Funding Project(No.2021YFS0221; No.2023YFS0179); 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (No.2022HXFH032; No.ZYJC21058); the Postdoctoral Research Funding of West China Hospital,Sichuan University, China (No.2020HXBH044).
Conflicts of Interest:Wang LX,None;Deng YP,None;Xie MZ,None;Ma K,None;Yin HB,None;Wang Q,None;Gong R,None;Tang J,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Meibomian glands segmentation in infrared images with limited annotation
- Artificial intelligence for the detection of glaucoma with SD-OCT images: a systematic review and Meta-analysis
- Overexpression of TRPV1 activates autophagy in human lens epithelial cells under hyperosmotic stress through Ca2+-dependent AMPK/mTOR pathway
- Dry environment on the expression of lacrimal gland S100A9, Anxa1, and Clu in rats via proteomics
- Semaphorin 7A impairs barrier function in cultured human corneal epithelial cells in a manner dependent on nuclear factor-kappa B
- Novel MIP gene mutation causes autosomal-dominant congenital cataract
