A systematic review of robot-assisted partial nephrectomy outcomes for advanced indications: Large tumors (cT2-T3), solitary kidney, completely endophytic, hilar,recurrent, and multiple renal tumors
Svo Domenco Pndofo , Cr Cerrto , Zene Wu ,Antono Frnco , Frncesco De Gudce ,Aessndro Scrr , Poo Verze , Guseppe Lucre ,Cro Immo , Ssto Perdonà , Edwrd E.Ceruo ,Frncesco Porp , Itr H.Derwees ,Rccrdo Autorno ,*
a Department of Urology, Rush University Medical Center, Chicago, IL, USA
b Department of Neurosciences, Reproductive Sciences and Odontostomatology, “Federico II”University, Naples, Italy
c Department of Urology, University of Verona, Verona, Italy
d Department of Urology, Changhai Hospital, Naval Medical University, Shanghai, China
e European Association of Urology(EAU)Young Academic Urologists(YAU)Renal Cancer Working Group,Arnhem, the Netherlands
f Department of Urology, Sant’ Andrea Hospital, La Sapienza University, Rome, Italy
g Department of Maternal-Infant and Urologic Sciences, La Sapienza University, Policlinico Umberto I Hospital, Rome, Italy
h Department of Medicine and Surgery,Scuola Medica Salernitana,University of Salerno,Fisciano,Italy
i Department of Emergency and Organ Transplantation-Urology,Andrology and Kidney Transplantation Unit, University of Bari, Bari, Italy
j Department Uro-Gynecology, IRCCS G.Pascale Foundation, Naples, Italy
k Department of Urology, San Luigi Gonzaga Hospital, University of Turin, Orbassano, Italy
l Department of Urology, University of California San Diego, La Jolla, CA, USA
KEYWORDS Robot-assisted partial nephrectomy;Complex renal mass;Solitary kidney;Larger tumors (cT2-T3);Endophytic and hilar mass;Recurrent tumor;Simultaneous and multiple tumor
Abstract Objective: Robot-assisted partial nephrectomy(RAPN)has become widely used for treatment of renal cell carcinoma and it is expanding in the field of complex renal masses.The aim of this systematic review was to analyze outcomes of RAPN for completely endophytic renal masses,large tumors(cT2-T3),renal cell carcinoma in solitary kidney,recurrent tumors,completely endophytic and hilar masses, and simultaneous and multiple tumors.Methods: A comprehensive search in the PubMed,Scopus,Web of Science,and Cochrane Central Register of Controlled Trials databases was performed in December 2022 for English language papers.The primary endpoint was to evaluate the role of RAPN in the setting of each category of complex renal masses considered.The secondary endpoint was to evaluate the surgical and functional outcomes.Results: After screening 1250 records,43 full-text manuscripts were selected,comprising over 8500 patients.Twelve and thirteen studies reported data for endophytic and hilar renal masses,respectively.Five and three studies reported outcomes for cT2-T3 and solitary kidney patients, respectively.Four studies focused on redo-RAPN for recurrent tumors.Two studies investigated simultaneous bilateral renal masses and five reports focused on multiple tumor excision in ipsilateral kidney.Conclusion: Over the past decade, evidence supporting the use of RAPN for the most challenging nephron-sparing surgery indications has continuously grown.Although limitations remain including study design and lack of detailed long-term functional and oncological outcomes, the adoption of RAPN for the included advanced indications is associated with favorable surgical outcomes with good preservation of renal function without compromising the oncological result.Certainly,a higher likelihood of complication might be expected when facing extremely challenging cases.However,none of these indications should be considered per se an exclusion criterion for performing RAPN.Ultimately, a risk-adapted approach should be employed.
1.Introduction
Renal cell carcinoma (RCC) represents a serious condition and its incidence in the United States alone was estimated to 79 000 new cases in 2022 and worldwide up to half a million [1,2].Partial nephrectomy (PN) has established itself as the preferred surgical option for clinical tumor stage 1 (cT1) and selected cT2 renal masses, whenever technically feasible [3-5].Current guidelines equally recommend open PN (OPN), laparoscopic PN (LPN), or robot-assisted PN (RAPN) [1,6].However, RAPN has been found to be an efficient alternative to OPN with lower perioperative complication rates, and demonstrated a shorter learning curve compared to LPN [7-9].
With the wide application of the robotic approach in the surgical treatment of RCC, the indication for nephron-sparing surgery (NSS) has been expanded to include the management of larger, deeper, and higher complexity renal tumors [10,11].
Considering the continuous evolution of current evidence, we aimed to summarize and analyze the outcomes of RAPN for most challenging indications including larger tumors (cT2-T3), RCC in solitary kidney (SK), completely endophytic and hilar masses, retreatment for recurrent localized renal tumor, and simultaneous and multiple tumors.
2.Materials and methods
A systematic review of the literature from January 2010 to December 2022 was performed using the PubMed, Scopus,Web of Science,and Cochrane Central Register of Controlled Trials databases.Preferred Reporting Items for Systematic review and Meta-Analyses (PRISMA) recommendations were followed to design the search strategies, selection criteria,and evidence report.The International Prospective Register of Systematic Review protocol number is CRD42023390374.Patient-related and intervention search terms were combined to build the following search string: ((robotic partial nephrectomy) OR (RAPN) OR (robot-assisted partial nephrectomy)) NOT (radical nephrectomy) AND ((complex renal masses) OR (complex kidney tumors) OR (cT2-T3) OR(endophytic) OR (hilar masses) OR (solitary kidney) OR(multiple renal masses) OR (simultaneous masses) OR(salvage robotic partial nephrectomy)).
Two authors (Pandolfo SD and Cerrato C) independently performed assessment of the titles and abstracts records gathered from initial literature search, and then evaluated full-text manuscripts to determine final inclusion.Any discrepancies were resolved by consultation with a third senior investigator (Autorino R).
Search results were filtered by language (English only),species (human), and publication type (original article).Study eligibility was defined using the PICOS (Patient,Intervention,Comparator,Outcome,Study type)approach.Inclusion criteria were: (1) Patients (P): studies focused on adults (>18 years of age) with a diagnosis of RCC; (2)Intervention (I): undergoing RAPN; (3) Comparator (C):OPN, LPN, or nothing was used as a comparator; (4)Outcome (O): evaluating one or more of the outcomes including perioperative outcomes (operative time [OT],estimated blood loss [EBL], warm ischemia time [WIT],major complication rate, and conversion rate), functional outcomes (estimated glomerular filtration rate [eGFR]preservation, upstaging chronic kidney disease [CKD], and trifecta achievement), and oncologic outcomes (positive surgical margin [PSM], recurrence rate, and metastases rate); (5) Study type (S): retrospective or prospective comparative studies, with a minimum cohort size of 10 patients.
Exclusion criteria were: (1) studies on animal or cadaveric models;(2)studies reporting fewer than five cases;and(3) non-original studies including editorial comments,meeting abstracts, case reports, or letters to the editor or any form of grey literature because of the general lack of details or peer review.
3.Quality assessment
This scoping review adopted the research design proposed by the A Measurement Tool to Assess Systematic Reviews-2(AMSTAR-2) guideline to inform the methodological and reporting process to ensure quality [12].Moreover, the quality of the studies included was determined using the Newcastle-Ottawa Scale for nonrandomized controlled trials [13].A total score of 5 or less was considered low quality;6-7 was considered intermediate quality;and 8-9 was considered high quality.This procedure was independently performed by two authors with disagreement resolved by consensus.
4.Literature search results
The PRISMA flow chart of the study selection process is shown in Fig.1.Initial search identified 1250 studies.Of these, 67 were excluded for duplication.After applying selection criteria, other 1140 records were excluded.A total of 43 studies including over 8500 patients, were included in the systematic review.
About 79% of the studies included were of high-quality scoring Newcastle-Ottawa Scale score of 8, and 21% recorded a score of 7 (Supplementary Table 1).
Twelve studies, including 2829 patients, reported data for completely endophytic renal mass [14-25] (Table 1).Thirteen studies,including 4881 patients,reported data on RAPN for hilar renal mass [26-38] (Table 2).Five retrospective studies with an overall of 588 patients reported outcomes for cT2-T3 renal masses[39-43](Table 3).Three retrospective multi-institutional series, with an overall of 187 patients, reported data on SK patients with renal masses [41,44,45] (Table 4).Four studies, including 124 patients, focused on redo-RAPN for recurrent localized renal tumor [46-49] (Table 5).Only two studies investigated simultaneous bilateral renal masses, total collecting 35 patients [50,51] (Table 6).Five reports, including 1268 patients, focused on multiple tumor excision in ipsilateral kidney [52-56] (Table 7).

Figure 1 The flow diagram for identification of studies via databases and registers [112].
5.Endophytic masses
Although there is no standardized definition, most studies identify endophytic masses as those scoring 3 points for the“E” domain of the R.E.N.A.L.nephrometry score, and more generally as those lesions completely covered by healthy parenchyma [15,57].The R.E.N.A.L.nephrometry score consists of(R)adius(tumorsizeasmaximal diameter),(E)xophytic/endophytic properties of the tumor, (N)earness of tumor deepest portion to the collecting system or sinus, (A)nterior(a)/posterior(p)descriptor,and the(L)ocation relative to the polar line.A completely endophytic lesion presents a challengingscenariotothesurgeonduetothelackofvisualclueand the large contact surface area between the tumor and normal parenchyma[24].
In this scenario, inaccuracy in tumor extension identification,increased risk of vascular injury,and the need for a reconstruction of parenchymal defect could negatively influence perioperative and oncologic outcomes and compromise renal function preservation [57].The lack of external visual cues of tumors on the kidney surface turns into the key role of preoperative imaging and intraoperative ultrasound.
Furthermore,the use of three-dimensional virtual models and augmented reality has been proposed to enhance the ability to provide better insight into the depth of the tumor and its relationship with the surrounding structures compared to two-dimensional images.These could become key instruments when facing such challenging scenarios[58-61].Furthermore, ultrasound can help localize and recognize the size and margins of non-palpable tumors and minimize PSM while retaining normal renal parenchyma.Intraoperative use of ultrasound has turned out to be the standard option for totally endophytic tumors [62,63].

Table 2 Outcomes of RAPN for hilar renal masses: overview of reported series.
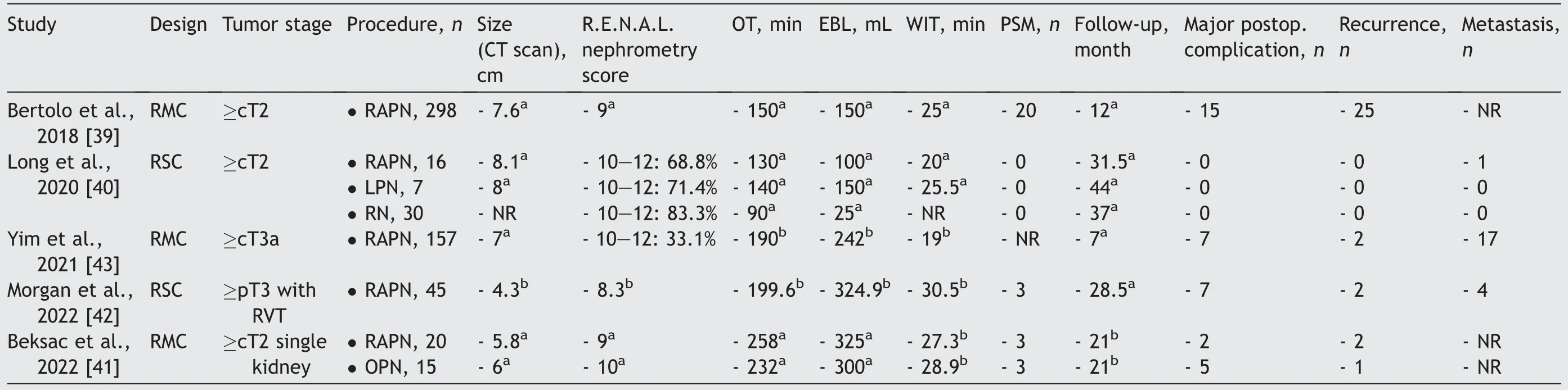
Table 3 Outcomes of RAPN for larger tumors (cT2-T3): overview of reported series.
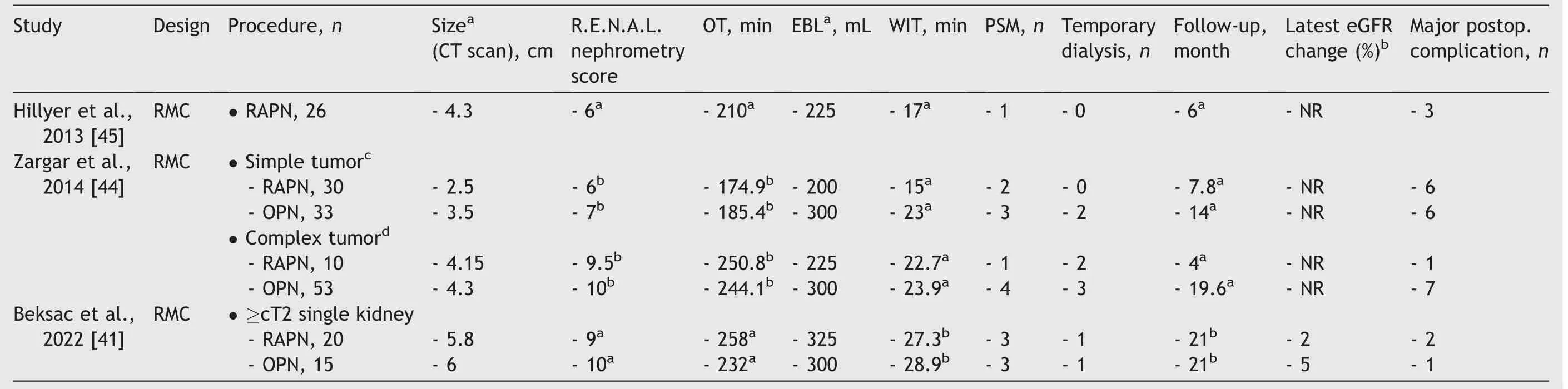
Table 4 Outcomes of RAPN for solitary kidney: overview of reported series.
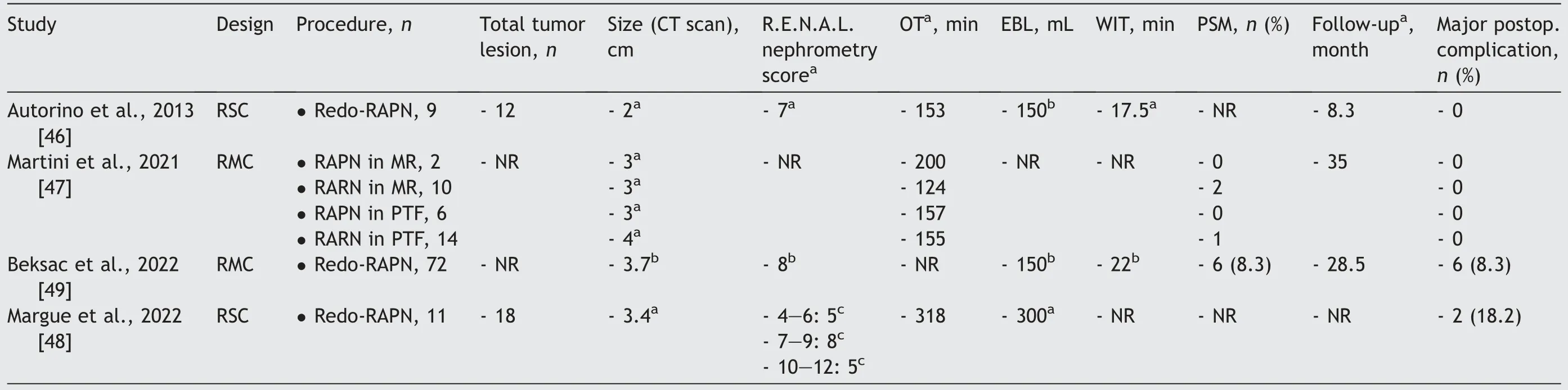
Table 5 Outcomes of RAPN for recurrent localized renal tumor: overview of reported series.

Table 6 Outcomes of RAPN for simultaneous bilateral tumors: overview of reported series.
Autorino et al.[19] presented the first single-center experience in this field with a comparison between endophytic,mesophytic,and exophytic masses,and showed the safety and feasibility of RAPN for endophytic renal masses with functional and oncological outcomes resembling those obtained in the general RAPN population.Since then,other three single-center experiences have been reported[14,23,24], confirming these findings.More recently,Carbonara et al.[16] reported the largest multicenter comparative analysis to date, confirming that RAPN in case of completely endophytic renal masses can be performed with acceptable outcomes, despite an increased risk of prolonged ischemia time and overall complications.
Minoda et al.[15] focused on comparison between enucleation and standard resection techniques.Authors reported better surgical outcomes for completely endophytic renal tumors in terms of preservation of renal function and OT than the standard resection technique without any significant difference in complication and PSM rates [64].
RAPN for endophytic mass was compared with OPN in different studies demonstrating equivalent long-term oncologic and functional outcomes [17], better trifecta achievement(75%vs.68.4%)[21],and shorter length of stay and less EBL for RAPN [20].When compared to LPN, RAPN offers a shorter learning curve while being more expensive[22].Abdel Raheem et al.[17] compared functional and oncological outcomes for RAPN versus OPN with a median 59-month follow-up.From a pathological standpoint, they reported PSM rates of 9.6% and 8.1% for RAPN and OPN,respectively.The rates are much higher compared with non-endophytic tumors, but it did not translate into higher recurrence rates.Moreover, Okhawere and colleagues [25]have recently demonstrated that transperitoneal and retroperitoneal RAPN yielded comparable perioperative and functional outcomes for patients with completely endophytic tumors.Focusing on the challenge of tumor localization, ultrasonography (US) had already been considered crucial for the LPN era[65,66].US provides realtime imaging which helps detecting and characterizing the anatomic relationship of the renal lesion to nearby structures, such as pelvicalyceal system renal sinus and renal vessels.The console surgeon-controlled“drop-in”US probe was even more valuable in achieving the appropriate angle while maintaining contact with the kidney surface [60,67].Sun et al.[18] reported that its use translates into lower EBL, shorter WIT, and lower surgical PSM rate.
6.Hilar masses
Hilar masses also represent a challenging surgical task,due to the proximity to the vessels and collecting system as well as the lack of hilar parenchymal tissue for the renorrhaphy.Therefore, highly complex hilar tumors have been traditionally treated via open surgery.We found one comparative study between RAPN and OPN[31].Indeed,Miyake and colleagues [31] reported how RAPN seems to result in favorable outcomes in terms of morbidity when compared to OPN, with oncological and safety equipoise.
With increasing experience,NSS approaches such as LPN,percutaneous ablation, and RAPN have become a more popular choice.With regard to ablative techniques,studies on radiofrequency and cryoablation for hilar RCC have reported higher rates of post-procedural tumor recurrence and complications for central compared to peripheral tumors while most promising initial results have been reported for microwave ablation[68].
More evidence is available on LPN which seems to be technically more complex compared to the robotic approach in achieving precise parenchyma resection and renal reconstruction in this demanding setting.Moreover,Gill et al.[69] showed the technical feasibility of LPN for renal hilar tumor, but higher complication rate was noted even in experienced surgeon.This is because LPN presents steep learning curves and needs more advanced surgical skills, especially for these renal hilar tumors.
We found one retrospective single center [32] and one multi-institutional prospective study [33], comparing RAPN with LPN.Hinata et al.[33] reported how the cohort of patients who underwent RAPN had significantly shorter WITs than a historical control values of LPN for cT1 renal hilar tumors.Both techniques had comparable PSM rates.
Dulabon et al.[38] reported the first multi-institutional analysis comparing the outcomes of RAPN for hilar masses versus non-hilar ones, and showed that RAPN is a safe,effective, and feasible option for the minimally invasive approach to renal hilar tumors, reporting longer mean WIT for hilar masses (26.3 min vs.19.6 min).In the hands of experienced robotic surgeons, there appears to be no increased risk of adverse outcomes compared with RAPN for non-hilar tumors.
Since then, other three single centers and one multicenter comparative reports have been published confirming these findings [26-29].Among those, Eyraud et al.[28]compared 70 hilar tumors with 297 non-hilar ones.The authors hypothesized that larger tumor size, higher tumor complexity, and the need for more careful vascular dissection translated into longer median OT (210 min vs.180 min) and median WIT (27 min vs.17 min) in the hilar arm.Indeed,location and size were independent predictors of WIT on multivariate analysis.This is consistent with the findings from the findings by Ficarra et al.[70] who found that higher PADUA classification score (preoperative aspects and dimensions used for an anatomical classification system) correlated to prolonged WIT.However, in most of these comparative reports, EBL was significantly higher for hilar tumors.Although statistically significant in most studies, the increase in EBL was not likely clinically significant considering the comparable transfusion rate between hilar and non-hilar tumors.Considering functional outcomes,Tyagi and colleagues[26]did not find differences in eGFR, CKD upstaging, or 90% eGFR preservation at 1 year.Lu et al.[29] did not record any significant difference in eGFR at 6 months and 12 months.Eyraud et al.[28]also did not note any difference in CKD upstaging and eGFR change.Despite the overall complexity due to the anatomical localization associated with longer WIT and increased EBL,all reports agreed on equal renal functional recovery when compared to non-hilar arms.This suggests that once a successful RAPN is performed,the tumor complexity due to hilar location itself will not affect the functional outcome.
Mellouki et al.[30] compared on-clamp with off-clamp approach, reporting similar PSM rates between the two groups.Similar findings were reported by Ferriero et al.[36] who showed excellent perioperative, oncologic, and functional outcomes for off-clamp RAPN.Those findings are consistent with the results of the CLOCK randomized trial[71] and the recent systematic review by Cacciamani et al.[72].
As mentioned above, following hilar tumor resection,the lack of viable renal parenchyma for the renorrhaphy might constitute a surgical challenge.Khalifeh et al.[37]proposed a “VHS” technique to elegantly overcome this issue.On the other hand, Gao et al.[34] proposed a“Garland” technique to allow a tension-free renorrhaphy technique when dealing with large parenchymal defects.Zhang et al.[35] assessed the clinical value of holographic imaging and navigation techniques in this setting.Finally,the recent introduction of technological advancements such as three-dimensional reconstruction and the use of intraoperative US are also gaining attention as crucial tools in this setting of patients [63].
7.Larger tumors (cT2-T3)
Current guidelines suggest a risk-adapted approach in the debate PN over radical nephrectomy (RN) in those challenging scenarios [1].Moreover, RN is still regarded as the reference standard for cT2 RCC[73,74].In fact, tumor size per se is no longer considered a contraindication to PN,and advancements in robotic techniques resulted in expanded indications to include selected cases of larger tumors(cT2-T3).
Ghali and colleagues [75] reported the largest comparison between OPN and RAPN for cT2a disease (RAPN 59 and OPN 91) and noted a significantly higher rate of trifecta achievement in the RAPN group.This was most likely driven by a lower major complication rate in the RAPN cohort,while negative margin or renal functional recovery rates were not significantly different.Taken together with well-described decreases in EBL and length of stay in favor of RAPN, those findings suggest that RAPN may be a first-line management approach [75].
The “ROSULA” collaborative group reported a large series of RAPN for cT2 renal masses and confirmed that the robotic approach allows acceptable WIT (25 min) and complication rates(21%overall and 5%major)[39]that are higher than those reported for RAPN for smaller masses[76], but lower than those reported for OPN in cT2 tumors[77,78].
Long et al.[40] reported comparison for cT2 RCC of RAPN to LPN and RN.Compared with radical surgery,PN can provide better preservation of renal function and no local recurrence was detected in all cohorts; the authors confirmed RAPN feasibility and effectivity for RCC of>7 cm.Moreover, Beksac et al.[41] focused on the comparison for RCC of OPN to RAPN in single kidney patients concluding that in select cases and experienced hands, the robotic approach offers a reasonable alternative to open surgery without compromising oncological and functional outcomes.
A cT3a RCC is defined as a mass that invades the renal vein or branches, perirenal sinus fat, or renal calyces [79].Compared to cT1 and cT2 RCC, this represents locally advanced disease with worse survival outcomes[80].In this scenario,the increased technical difficulty is related to the concern about the resection margin status and the potentially prolonged clamping time [81].However, Yim et al.[43] reported a multi-institutional analysis from the ROSULA group, showing similar PSM and complication rates of RAPN for cT2-T3 renal masses compared to RAPN for lower stage tumors [39,82].Moreover, eGFR preservation and survival were similar to those reported for OPN in cT3a RCC[83].The study of Morgan and colleagues[42]included only patients with renal vein thrombus,and concluded that renal vein thrombus does not preclude RAPN which appears viable treatment for selected cT3a RCC patients.
8.SK
SK has been traditionally considered an imperative indication for NSS, and OPN the gold standard NSS procedure for this indication [36].Other minimally invasive NSS options have been proposed including LPN and percutaneous ablation (PTA).While LPN demonstrated comparable indication and outcomes [84], PTA is recommended by the guidelines for selected patients with a small renal tumor (<3 cm),especially in frails unfit for PN.Recently, a large comparative analysis between RAPN and PTA for SK patients found no significant difference between the two cohorts in eGFR drop after 1 year and at the latest follow-up.Moreover, in the same study, no statistically significant difference in recurrence rates between PTA and RAPN(6.7%vs.4.0%)was found.On the other hand, the Kaplan-Mayer analysis showed a shorter recurrence-free survival for the PTA,which might suggest earlier recurrences in this group [80].Subsequent reports on PTA demonstrated good oncologic outcomes in the management of SK patients, but a higher risk of recurrence when compared with RAPN.However,retreatment is possible [85,86].The rationale behind the choice of RAPN over other PTA techniques could be driven by the patient’s comorbidities and the eligibility for surgery.
Focusing on the robotic approach only, there is ample literature supporting the role of RAPN in this setting.Hillyer et al.[45] reported the first multi-institutional series of RAPN in SK patients with small renal masses.Early in the RAPN experience, a comparative series was reported by Zargar et al.[44] who divided tumors according to R.E.N.A.L.nephrometry score.For less complex(R.E.N.A.L.nephrometry scores 4-8) ones, RAPN and OPN were comparable in terms of PSM, complication rate, and functional outcomes.They observed the same findings for more complex lesions (R.E.N.A.L.nephrometry scores 10-12).A larger comparative analysis was more recently reported by Beksac et al.[41] who focused on SK patients with cT2-T3 RCC disease.Even in this challenging setting, RAPN yielded comparable outcomes to OPN.
In SK patients, special emphasis is on functional outcomes, where preoperative healthy nephron reserve is lower and the detrimental effect of postoperative renal functional recovery is more prominent [87].Acute kidney injury (AKI) following PN poses an increased complication risk,end-stage renal disease,and subsequent dialysis which pave the way for cardiovascular events, hospitalization,and all-cause mortality [88].In the report by Beksac et al.[41],both arms had low baseline eGFR,but only one patient for each group required temporary dialysis while eGFR preservation rate at the last follow-up was 79.1%.Hillyer and colleagues [45] classified CKD Stage 3 as the predominant postoperative phase, with Stage 2 observed in eight patients and Stage 4 in five patients.Importantly, none of the individuals necessitated dialysis.Zargar et al.[44]described a slight advantage of RAPN over OPN in low-complex settings (R.E.N.A.L.nephrometry scores 4-8)in terms of temporary dialysis required (with 0 vs.2 patients), while overlapping results were twisted in the setting for more complex lesions (R.E.N.A.L.nephrometry scores 10-12) (2 vs.3 patients).
A large meta-analysis conducted by Pierorazio et al.[89]showed that PTA has better perioperative functional outcomes compared to PN.Moreover, in patients undergoing treatment for a renal mass suspicious for clinical stage T1 or T2 RCC, kidney function consistently worsened in the immediate postoperative setting, but improved during the next 1-6 months and remained relatively stable after that point.This improvement was more pronounced in thermal ablation arms.In addition, patients with optimal baseline renal function (eGFR>90 mL/min/1.73 m2) experienced less decline in eGFR.This suggests that PTA could be considered a valid therapeutic option.
9.Redo-RAPN for recurrent localized renal tumor
Despite being uncommon, local recurrence is an adverse outcome that occurs in 1%-10% of renal cancer patients after PN or ablative therapies [90].
Results of several large retrospective studies showed that the progression rate after PN versus RN was similar and depended on the features of the tumor, rather than the surgical procedure [91].This is easily acceptable in case of distant metastases because micrometastasis is not amenable to being cured by any local treatment.Conversely, in case of a relapse in the same kidney submitted to PN,some concerns on the primary procedure can be raised.
However, it is difficult to distinguish between different biological entities.Moreover,local recurrence can occur as a metachronous lesion in the same kidney outside the resection bed, such as new oncologic event, or as a persistence of disease in the resection bed after prior treatment, representing its failure.
Clinical decision-making in this setting is a clinical challenge.When opting for re-operation,the surgical field is not na?¨ve,and this might increase the technical complexity and complication risk.Moreover, technical-specific challenges of performing RAPN for recurrent renal tumors are mostly related to the presence of previous abdominal scars,requiring meticulous lysis of intra-abdominal adhesions.Transperitoneal access through the most geographically distant quadrant is needed to avoid injury to adjacent organs and significant hemorrhage.Furthermore, dense adhesions around the hilum are expected if previous hilum dissections have been performed and vessel accurate dissection is required to fibrous tissue encasing the renal vein.
Prior OPN poses a different technical challenge.Owing to the adhesions, establishing pneumoperitoneum can be difficult, and lysis of adhesions may pose additional challenges intraoperatively and postoperatively.Autorino and colleagues [46] reported a preliminary series of redo-RAPN cases of 12 patients in the past, with effective attempts in five patients with failed previous OPN.Gurram and colleagues [92] published 47 effective RAPN cases after prior OPN.However, the significant majority of their cohort consisted of hereditary forms of RCC.It is likely that the majority of their cohort was made up of metachronous renal masses as opposed to the recurrent renal masses in our cohort.In any case, their series demonstrated the feasibility of RAPN after previous ipsilateral OPN.
Although RN has been traditionally considered reasonable in this challenging setting, repeat PN may still be the preferred option, as it maximizes renal function preservation [93].
Autorino and colleagues [46] showed for the first time the feasibility of RAPN for ipsilateral recurrent renal tumors.The most common previous ipsilateral NSS procedure was OPN (five patients) and the median time from the previous NSS procedure was 39.4 months.Subsequently,Martini et al.[47] in a multi-institutional collaborative dataset by the Junior European Association of Urology(EAU) Robotic Urology Section/Young Academic Urologists Working Group classified the treatments and standardized the nomenclature of salvage robot-assisted renal surgery.The authors concluded that in the case of prior RN, the rates of RAPN and robot-assisted radical nephrectomy were 25% and 75%, respectively; in seven of those patients who received robot-assisted radical nephrectomy, PN was planned, but radical surgery was carried out due to complexity [47].In this view, salvage robot-assisted renal surgery includes multiple and heterogeneous scenarios that should be precisely classified according to the type of primary treatment.Indeed, a recent multi-institutional study reported that the rate of PSM was 8.5% after savage RAPN;however, their cohort had a relatively high ratio of hilar tumors(20.6%)versus SKs(9.7%).Functional outcomes were promising as 78%eGFR was maintained at discharge and 90%maintained at 1-year follow-up [49].Finally, Margue et al.[48]focused on true salvage indications where patients had ablative treatment failure.The authors reported trifecta achievement in five patients (45.5%) and the modified NSS composite outcome in three (27.3%), and more generally good functional and short-term oncological outcomes.
10.Simultaneous bilateral tumors
Bilateral renal tumors account for around 3% of renal tumors [94].Hereditary bilateral renal tumors display different biological behaviors from bilateral synchronous renal tumors [95].Surgery is the gold standard for treating bilateral sporadic renal tumors since its prognosis is comparable to unilateral sporadic renal tumors.However,when bilateral RN is performed, dialysis becomes most likely after surgery.Therefore, bilateral PN represents an absolute indication due to their high rates of tumor recurrence, need for repeat PN, and risk of long-term renal replacement therapy [96].
Even if the robotic approach is emerging as an attractive minimally invasive NSS technique for all complex renal tumors, alternative approaches are available, as long as the goals remain oncologic control and renal functional preservation.Moreover, Hillyer and colleagues [97] reported a comparison between LPN and RAPN in patients with bilateral synchronous renal tumors describing that as the complexity of the tumors increased, the WIT, EBL, and OT increased in the LPN compared with the RAPN group.Instead, Zhang et al.[98] reported encouraging outcomes in a case series where patients were treated with radiofrequency ablation for synchronous bilateral RCC.The local tumor control rate was 93.1% and the latest mean eGFR had not significantly declined compared with preoperative levels [98].
The decision to perform a simultaneous bilateral surgery or a two-step surgery is based on surgeon experience and center volumes.However, the superiority of either the simultaneous or sequential procedure for bilateral renal tumors is still debated.The Mayo Clinic reported 76 cases,including 75 laparotomy cases and one LPN case, treated with simultaneous bilateral PN [96].Around 10.8% of cases experienced AKI during the perioperative period,but there were no patients requiring dialysis.The authors reported a median decrease in eGFR values of 19 mL/min/1.73 m2[96].They recommended staged procedures for patients with bilateral synchronous sporadic renal tumors and impaired renal function.Moreover, Lowrance et al.[99]reported that the sequential procedure could minimize renal dysfunction, and patients could avoid dialysis treatment.Overall, the simultaneous procedure may be prioritized if technically feasible because of the merit of reducing hospitalization costs and completing the procedure with only a single general anesthesia.However, only a few data on simultaneous NSS were available [100].A pilot experience from Otoshi et al.[50]reported results on eight patients with eighteen tumors with no PSM and one AKI,suggesting that simultaneous RAPN for bilateral renal tumors may be feasible.Gallo and colleagues[51] reported a wider Italian multicenter experience.All bilateral PNs were performed in 27 patients with median results on OTs,WITs,and EBLs consistent with literature [101].Along with favorable preoperative patient characteristics (favorable body mass index [27 kg/m2], low American Society of Anesthesiologists scores [1 and 2 in 74% patients], low Charlson comorbidity score[≤3 in 85.2%patients],and sufficient renal function [86.7 mL/min]), the main surgical selection criteria were represented by the high likelihood to avoid bilateral main artery clamping in the preoperative planning.In fact, complete clamping of both arteries could be avoided in four cases,and main or elective artery clamping was performed in 50% of procedures with a median WIT of 15 min.An expected eGFR decrease occurred with value improvement during the follow-up without any AKI.Concerning postoperative complications, the increased risk of postoperative renal hemorrhage may be a concern.Overall complication rate was 25.9% with only 3.7% being major complications.Similar complication rates have been reported for unilateral or bilateral simultaneous procedures[5,100,102].Concerning oncologic aspect, PSM (3.7%) was similar to those reported for RAPN for sporadic tumors[24,83,103].Based on these aspects,the authors concluded that simultaneous bilateral PN in the hands of expert surgeons is feasible.
11.Multiple ipsilateral tumors
The incidence of ipsilateral synchronous multifocal masses can be as high as 25%[104].Although current guidelines do not address their specific management, RN has been regarded as the standard treatment.Unfortunately, patients with ipsilateral synchronous renal masses would be highly predisposed to form contralateral renal tumors at the morbidity of about 5% compared to patients with unilateral renal mass [105]; thus NSS has been taken into consideration balancing oncologic effectiveness with renal functional optimization.
To date, diagnostic imaging is still the mainstay of surgical planning.However, no standardized management for multifocal masses based on preoperative imaging does currently exist.A clinical proxy for the number of mass excisions eventually performed is needed and several factors would be important to consider, including the number and size of ipsilateral renal masses, the proximity of one mass to another, and the likelihood of having to perform one excision versus multiple.Intraoperatively,laparoscopic ultrasound guidance should be considered a standard tool in this setting, and surgical extirpation is routinely initiated beginning with smaller exophytic lesions and progressing to larger and deeper tumors [54,106].
Among NSSs, Lin et al.[107] reported comparable renal functional outcomes, complication rates, and intermediate-term survival rates of 27 patients treated with LPN or cryoablation for synchronous multiple ipsilateral renal tumors in a single operating session.RAPN also has been shown to be effective in this setting and could greatly help to overcome laparoscopy challenges because of its technical advantages which can facilitate the identification of small branches of the renal arteries in case of selective clumping and more precise operating angle that can realize the quick resection and renorrhaphy of multiple lesions [108].The included studies have shown the transperitoneal approach as the preferred method in this setting and surgical extirpation was usually initiated beginning with smaller exophytic lesions and progressing to bigger and deeper ones.Historically, patients with hereditary renal disease are carefully monitored and progress to surgery when the largest tumor reaches 3 cm in size [109].Laparoscopic ultrasound guidance is used routinely in almost all cases to define tumor number and localization and has also been used to identify renal vasculature for selective clamping and determine the distance between tumor and segmental vessels.In cases with renal vein and inferior vena cava thrombi, ultrasound can help localize the proximal extent of thrombus [18,67].Laydner and colleagues[110] reported an early case series of sporadic ipsilateral multifocal renal tumors showing RAPN feasibility and safety in this setting; even off-clamp resection can be safely performed in carefully selected lesions.Boris et al.[54]presented an early experience of removing 24 tumors in 10 patients demonstrating how RAPN for multiple renal masses is safe and feasible in their early experience.Renal functional outcome was minimally affected with a limited follow-up of 9.4 months.According to the anatomic characteristic,Yang et al.[55],in order to further optimize the surgery treatment,proposed a novel clamping procedure of lesion-feeding arteries, by sequential clamping of precise segmental renal arteries during RAPN to avoid longer WIT of any spared nephrons for more than 20 min; although the mean of total WIT was 37.5 min, the mean clamping time for single lesion was only 18.8 min.
A comparative analysis for unilateral, synchronous, and multifocal renal tumors using either an open or robotic approach was performed by Yerram and colleagues [56].RAPN achieved equivalent rates of trifecta to open surgery(14.7% vs.17.0%, p=0.83), which persisted on subgroup analyses of patients with two(20.8%vs.23.9%,p=0.84)or more than two tumors(4.3%vs.7.0%,p=0.74).The robotic cohort had a shorter mean length of stay compared to open approach (3.7 days vs.5.0 days, p<0.001) and lower EBL(280 mL vs.357 mL, p=0.33) [56].Moreover, Hankins and colleagues [52] presented functional outcomes after RAPN on SK for more than three renal masses.They mostly performed off-clamp procedures achieving higher EBL with good preservation of renal function.Concerning the complication rate, Maurice et al.[53] reported a stratified analysis based on the number of multiple ipsilateral masses; RAPN involving more than two excisions was associated with a >20% overall compilation rate and >10%higher risk of major complications.These findings are expected as one would think that multiple excisions might potentially increase morbidity.
12.Limitations and future perspectives
The present study is not devoid of limitations.Selection bias cannot be ruled out given the retrospective design of most studies.No randomized controlled trial and only one prospective multicenter study have been included.Given the diversified nature of all scenarios included,the studies were short of important functional outcomes, resulting in the inability to provide all outcomes for each study, which may limit the strength of our evidence.Most of the data and patients included for uncommon and infrequent indications such as simultaneous bilateral tumors or multiple ipsilateral tumors come from little series, which leads to the lack of detailed and long-term functional and oncological outcomes.Thus, large-scale multicenter clinical studies are still needed to further prove the advantages of RAPN in all the explored settings.Given the comprehensive report of all the most complex scenarios in renal masses management,we believe there is significant utility in our study.
Overall,prospective multicentric studies with long-term follow-up and randomized controlled trials are needed to further validate the advantages of RAPN.Future research efforts should be also focused on the comparison between RAPN and other NSS options to further elucidate the optimal management strategy for these complex cases.Specifically, cost-effectiveness along with surgeon experience and the related learning curve of each NSS approach could be also examined.In addition, developing a standardized system for each of the challenging indications reporting may be useful.Several factors would be important to consider, including tumor characteristics, such as size, location, and histology, and whether there are any specific patient subgroups that may be more suitable candidates for this approach.
Last,one should consider that in the settings of complex renal masses, new technologies may play a significant role[59,106,111,112].Continuous technologic advancement and refinement of techniques including the use of augmented reality, novel ultrasound techniques, changes in surgical approach and reconstruction, and implementation of early recovery after surgery protocols might become key instruments when facing such challenging scenarios [58-61].Preliminary data suggest that pre-and peri-operative use of three-dimensional models may maximize renal function preservation, adding a novel tool to further enhance functional NSS outcomes [56,58].
13.Conclusion
Over the past decade,evidence supporting the use of RAPN for the most challenging NSS indications has continuously grown.Limitations remain, most studies being retrospective, often lacking a detailed and long-term reporting of functional and oncological outcomes,and only coming from high-volume centers.Nevertheless, the adoption of RAPN for these advanced indications is associated with favorable surgical outcomes with good preservation of renal function without compromising the oncological result.Certainly, a higher likelihood of complication might be expected when facing extremely challenging cases.However,none of these indications should be considered per se an exclusion criterion for performing RAPN.Ultimately, a risk-adapted approach should be implemented, considering patient and tumor factors, and also considering surgical expertise.
Author contributions
Study concept and design: Savio Domenico Pandolfo, Clara Cerrato, Zhenjie Wu, Antonio Franco, Riccardo Autorino.Data acquisition: Savio Domenico Pandolfo, Clara Cerrato.Data analysis: Savio Domenico Pandolfo, Clara Cerrato,Zhenjie Wu, Antonio Franco.
Drafting of manuscript:Savio Domenico Pandolfo,Riccardo Autorino.
Critical revision of the manuscript: Savio Domenico Pandolfo, Clara Cerrato, Zhenjie Wu, Antonio Franco, Francesco Del Giudice, Alessandro Sciarra, Paolo Verze,Giuseppe Lucarelli,Ciro Imbimbo,Sisto Perdonà,Edward E.Cherullo,Francesco Porpiglia,Ithaar H.Derweesh,Riccardo Autorino.
Conflicts of interest
The authors declare no conflict of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2023.06.001.
 Asian Journal of Urology2023年4期
Asian Journal of Urology2023年4期
- Asian Journal of Urology的其它文章
- Robot-assisted adrenalectomy: Step-by-step technique and surgical outcomes at a high-volume robotic center
- The application of internal suspension technique in retroperitoneal robot-assisted laparoscopic partial nephrectomy with a new robotic system KangDuo Surgical Robot-01: Initial experience
- Three-dimensional automatic artificial intelligence driven augmented-reality selective biopsy during nerve-sparing robot-assisted radical prostatectomy:A feasibility and accuracy study
- First 100 cases of transvesical single-port robotic radical prostatectomy
- Robot-assisted oncologic pelvic surgery with Hugo?robot-assisted surgery system: A single-center experience
- Prospective observational study on the prognosis of ureteral lesions caused by impacted stones via dual-energy spectral computed tomography
