First 100 cases of transvesical single-port robotic radical prostatectomy
Roxana Ramos-Carpinteyro, Ethan L.Ferguson, Jaya S.Chavali,Albert Geskin, Jihad Kaouk*
Glickman Urological & Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH, USA
KEYWORDS Prostate cancer;Radical prostatectomy;Robotic-assisted surgery;Single-port;Minimally-invasive surgery
Abstract Objective: To describe the surgical technique and report the early outcomes of the transvesical (TV) approach to single-port (SP) robot-assisted radical prostatectomy.Methods: All procedures were performed at a single center by one surgeon.We identified the first 100 consecutive patients with clinically localized prostate cancer that underwent SP TV robot-assisted radical prostatectomy using the da Vinci SP robotic surgical system.Data were collected prospectively and analyzed with descriptive statistics.The primary outcomes assessed were postoperative urinary continence, rate of biochemical recurrence, and sexual function.Results: All procedures were performed without extra ports or conversion.The median age was 62.1 years and 49.0%of the patients had abdominal surgery history.The preoperative median prostate-specific antigen value and prostate volume were 5.0 ng/mL and 33.0 mL,respectively.There were no intraoperative complications.The median operative time and estimated blood loss were 212.5 min and 100.0 mL, respectively.A total of 92.0% of patients were discharged within 24.0 h, with an overall median length of stay of 5.6 h.Only 4.0% of patients required opioid prescriptions at discharge.The median Foley catheter duration was 3 days.Positive margins were present in 15.0% of cases.Median follow-up was 10.4 months.Continence rate was immediate after Foley removal in 49.0% of cases, 65.0% at 2 weeks, 77.4% at 6 weeks, 94.1% at 6 months, and 98.9% at 1 year.One case of biochemical recurrence (1.0%)was noted 3 months after surgery.Conclusion: The SP TV approach for radical prostatectomy cases is a safe and feasible technique for patients with clinically localized prostate cancer.This technique offers advantages of short hospital stay,minimal narcotic use postoperatively,and promising early return of urinary continence, without compromising oncologic outcomes.
1.Introduction
Radical prostatectomy is a first-line treatment for clinically localized prostate cancer, especially in patients with favorable intermediate-risk, and unfavorable intermediate- or high-risk disease with an estimated life expectancy greater than 10 years, according to the National Comprehensive Cancer Network risk stratification [1-3].Robot-assisted radical prostatectomy (RARP) has demonstrated oncologic,sexual, and urinary continence outcomes similar to open surgery, and it is now the most used technique in many countries [4,5].While the transperitoneal approaches have dominated the literature over the last two decades, several other approaches have been described, including perineal,extraperitoneal, and transvesical (TV) [6-8].
The single-port (SP) surgical system was developed in 2018 and has been adopted for radical prostatectomy [9].The SP TV RARP was first shown to be technically feasible in a preclinical model and has been associated with faster recovery and improved time to continence in its initial study [8].The approach has the additional benefits of minimizing narcotic requirements and the ability to gain safe access to the bladder in patients with a hostile surgical abdomen, in whom minimally-invasive radical prostatectomy may otherwise be contraindicated.
This study described the technique, reported the outcomes, and highlighted the advantages of the first 100 SP TV RARP cases performed at our center.
2.Patients and methods
The procedure and prospective data collection were approved by the Institutional Review Board (No.5341).The first consecutive 100 SP TV RARP cases done in our center occurred from November 2020 to March 2022.All the surgeries were performed by the same surgeon(Kaouk J)using the da Vinci SP robotic surgical system (Intuitive Surgical,Inc., Sunnyvale, CA, USA).Patients with a history of extensive abdominal surgeries (hostile abdomen) and/or clinically localized and intermediate- to very high-risk prostate cancer were considered suitable for the procedure.Prostate volume greater than 80 mL on preoperative imaging was considered a relative contraindication for the TV approach.Specific cases of very low- to low-risk were also included if they had a strong family history of prostate cancer, or if they preferred this approach.The initial risk stage was established according to the National Comprehensive Cancer Network risk stratification [3].The Briganti nomogram was used to predict the risk of lymph node involvement.Patients with more than 7% risk were candidates for limited lymph node dissection during the same surgical event [10].
2.1.Variables
Demographic and baseline pathological characteristics were assessed.Perioperative variables of interest included operative time, estimated blood loss, and intraoperative complications.Postoperative outcomes such as length of hospital stay and complications (assessed through Clavien-Dindo stratification), need for pain medication at discharge, and time to catheter removal were analyzed.The surgical specimens were sent for pathological diagnosis.The main outcomes studied were those related to long-term follow-up and included time to continence, sexual function, and oncologic biochemical recurrence (BCR).Follow-up appointments at 1 week, 2 weeks, 6 weeks, 3 months, 6 months, and 1 year were analyzed.Time to continence was assessed through the need for incontinence pads; zero to one pad for protection was considered a continent patient.Sexual function was assessed with the Sexual Health Inventory for Men (SHIM) tool.A prostate-specific antigen(PSA) of more than or equal to 0.2 ng/mL in subsequent measurements was considered BCR.
2.2.Statistical analysis
Data were collected prospectively and analyzed using descriptive statistics: frequencies, measures of central tendency, and measures of variability, according to the type of variable.Learning curve was measured with time and analyzed with the cumulative sum method [11].All analyses were done using Microsoft Excel (Microsoft Corporation,Redmond,WA,USA)and SPSS Statistics version 25(IBM, Armonk, NY, USA).
2.3.Surgical technique
The technique described has been enhanced since the initial cases were performed [8].Changes made are addressed in the discussion section.
2.3.1.Preparation
After general anesthesia was achieved, the patient was placed in a supine position and little to no Trendelenburg inclination was needed (Fig.1A).Points of pressure were padded accordingly.A 20 French Foley catheter (Covidien,Dublin, Ireland) was inserted through the urethra and the bladder was filled with approximately 200.0 mL of saline solution for identification.

Figure 1 Patient preparation.(A) Dorsal decubitus position,parallel to the ground;(B)Suprapubic midline single incision of 3.5 cm.
Port access was obtained through a 3.5 cm suprapubic midline incision done about two fingerbreadths superior to the pubic symphysis (Fig.1B).This incision went through the skin, subcutaneous tissue, and anterior rectus fascia.The bladder was then identified by aspirating 5.0 mL of urine with a 21-gauge needle syringe.A 2.0 cm midline vertical cystotomy was made.Then, the da Vinci SP access port (Intuitive Surgical Inc., Sunnyvale, CA, USA) was introduced.This access port was composed of an Alexis wound retractor(Applied Medical,Rancho Santa Margarita,CA,USA), a transparent chamber(bubble), with entry sites for robotic instruments, insufflation, and the remotely operated suction and irrigation system (Vascular Technology, Nashua, NH, USA).The robot was docked (Fig.2).An 8.0 mm AirSeal port (CONMED, Utica, NY, USA) was used to insufflate the bladder to no more than 12.0 mmHg(1.0 mmHg=0.133 kPa).The rest of the instruments were inserted through the channels as follows: camera superiorly, Cadiere forceps inferiorly, monopolar curved scissors in the right, Maryland bipolar forceps in the left, and the remotely operated suction and irrigation in its designated port.
2.3.2.Console time
The bladder neck dissection started posteriorly in a semicircular fashion, carefully avoiding the ureteral orifices(Fig.3A and B).Once the vas deferens and the seminal vesicles were reached, the vas deferens was transected,and the seminal vesicles arteries were clipped with a medium-large Weck Hem-o-lok ligation system (Teleflex,Wayne, PA, USA) bilaterally (Fig.3C and D).The posterior plane was achieved through the incision of the rectoprostatic fascia and continued towards the prostatic apex.
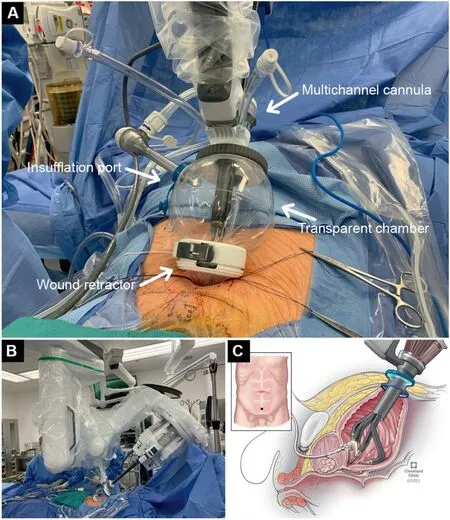
Figure 2 Access port and robot docking.(A) Da Vinci SP access port; (B) Docked robot; (C) Robot inside bladder illustration.
The anterior dissection started with incision of the remaining bladder neck attachments.The endopelvic fascia and puboprostatic ligaments were identified and incised(Fig.3E).The anterior plane was established between the prostate and the dorsal venous complex, sparing the retropubic (prevesical) space of Retzius.Openings in the dorsal venous complex are ligated with a 3-0 V-Loc barbed suture device (Covidien, Dublin, Ireland) and the vascular pedicles are controlled with bipolar energy and/or surgical clips (Fig.3F-H).Nerve spare may be performed at this point, if planned.The urethra was identified and transected with maximal length preservation (Fig.3I).After the urethra was incised and apical attachments were released,the prostate was pulled into the bladder (Fig.3J).
When indicated, limited lymph node dissection was performed bilaterally by exerting lateral traction on the bladder neck opening,identifying the obturator nerve,and excising the visible external iliac lymph nodes (Fig.3K).Next,the bladder insufflation was decreased to 5-8 mmHg to reduce tension for the vesicourethral anastomosis.The vesicourethral anastomosis started at 6 o’clock and continued in a latero-superior direction, using one 3-0 V-Loc barbed suture device for each side (Fig.3L and 3M).The sutures met and were tied together at 12 o’clock.The Foley catheter was inserted into the bladder and the balloon was filled with 10.0-15.0 mL of sterile water(Fig.3N).The robot was undocked.The specimen was extracted through the SP and sent for pathological analysis.
2.3.3.Closure
The bladder was closed in two layers using 2-0 Vicryl sutures (Ethicon Inc., Raritan, NJ, USA).Abdominal layers were anatomically closed using size 0 Vicryl or polydioxanone sutures (Fig.4).
3.Results
Demographic and baseline characteristics could be found in Table 1.Comorbidities were present in 52.0% of the patients, with hypertension (46.0%), dyslipidemias(33.0%), and diabetes mellitus (14.0%) being the most frequent.Almost half of the patients(49.0%)had a history of abdominal surgery of open (27.0%), laparoscopic(11.0%),or both(11.0%)approaches.The median PSA level and prostate volume were 5.0 ng/mL and 33.0 mL,respectively.Most cases (71.0%) were intermediate- or high-risk localized disease.None of the patients in the series had a history of prior prostate interventions.Preoperatively 58.0% of patients were sexually active; 33.0%had moderate to severe erectile dysfunction (ED); and 6.0% were taking erection-enhancing medications.
All cases were consecutive and successfully performed without intraoperative complications, open conversion,placement of extra ports, postoperative drain, or blood transfusions.Relevant perioperative outcomes are summarized in Table 2.The median operative time and console time were 212.5 min and 133.9 min, respectively.Estimated blood loss ranged from 10.0 mL to 350.0 mL,with a median of 100.0 mL.
Postoperatively, complications occurred in 16 (16.0%)patients, of which 12 were low grade (Clavien-Dindo I).Urinary retention (9.0%), gastrointestinal (1.0%), and urinary tract infection(1.0%)were the most common of these complications.Two (2.0%) patients with lymphoceles required drain insertion not under general anesthesia(Clavien-Dindo IIIa).
Eighty of 87 (92.0%) patients that had a planned outpatient procedure left the hospital within 24.0 h.The median length of stay was 5.6 h.Inpatient cases were discharged within 30.0 h after surgery.A total of six (6.0%) patients were readmitted within the first week after surgery.Almost half of the patients(47.0%)did not require pain medications at all on discharge.Of those discharged with pain medications, 49.0% were discharged on nonsteroidal antiinflammatory drugs and 4.0% were prescribed opioids only.Foley catheters were removed during the first postoperative week in 95.0%of patients,with a median duration of 3 days.Urinary retention after catheter removal occurred in the nine (9.0%) patients mentioned above and all resolved with catheter re-insertion and void trial after 48.0 h.

Figure 4 Postoperative scar.
Pathological analysis demonstrated a median prostate specimen weight of 40.0 g.A total of 38 patients showed extra-prostatic extension, focal (<3.0 mm) in 12 patients,and 15.0%of specimens had positive margins.Invasion rates of the bladder neck, lymphovascular structures, and seminal vesicles were seen in 6.0%,7.0%,and 7.0%of specimens,respectively.Of the 29 patients with Gleason score 6 on biopsy, 25 of 29 (86.2%) patients with Gleason score 6 on biopsy were upgraded to Gleason score 7 on final pathology.
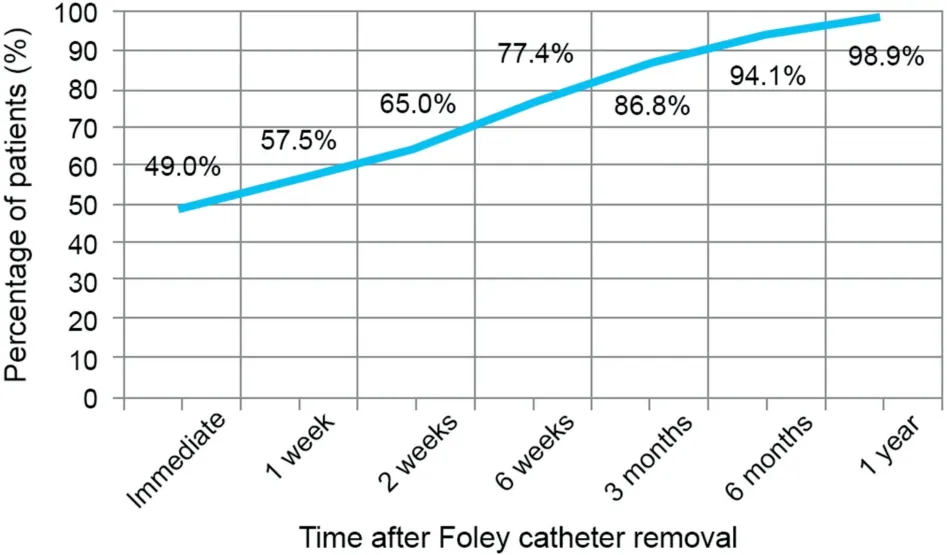
Figure 5 Percentage of continent patients after transvesical single-port robot-assisted radical prostatectomy.
Median follow-up was 10.4 months.The median time to continence(50.0%of patients)was 3 days,considering three outliers that obtained continence more than 1 year after surgery (Fig.5).Stress incontinence was diagnosed postoperatively in five cases within the first year of follow-up.Four of these patients were managed with pelvic floor physical therapy; the one with persistent stress incontinence required a sling.Median SHIM score was 5.0 at 6.0 weeks postoperatively, and for the patients with more than 6 months of follow-up (n=46), 17 (37.0%) reached more than 10 points(mild to moderate ED).Improvement in sexual function was seen with consequent visits(Fig.6).BCR occurred in one patient with PSA values of 0.2 ng/mL 3 months and 0.4 ng/mL 6 months after the surgery.
4.Discussion
In this study,we presented the updated outcomes for SP TV RARP.The greatest advantage of the TV approach is regionalization of treatment to the bladder and prostatic fossa,sparing manipulation of the retropubic space and the peritoneal cavity.The SP is a purpose-built robot that can work comfortably inside the bladder through a single 3.5 cm incision.Moreover, the initial selection of patients with a complex history of abdominal and pelvic surgery has broadened to include nearly all patients with clinically localized disease.
The surgical technique described in this paper is the culmination of a four-year process.Since 2018, work has been conducted on the SP robot in our center to think of innovative and beneficial approaches to common urological procedures.The TV approach was firstly described for robotic simple prostatectomy and then adapted for radical prostatectomy [7].Aside from obvious differences in access, bladder neck dissection, and the urethrovesical anastomosis, the surgical steps are similar to other approaches to transperitoneal RARP.Though the experience is limited to a single experienced surgeon, we expect a reasonable learning curve for other robotic surgeons.The specific steps have changed minimally, mostly in regard to closure materials used.
One of the recent improvements for this procedure is the access port design.Initially, a GelPOINT Mini Advanced Access Platform (Applied Medical, Rancho Santa Margarita,CA, USA) was used instead of the transparent chamber [8].The GelPOINT required an extra port through the gel for graspers, irrigation, and suction.The new SP access port was designed for the TV approach, so it includes a port for these instruments and it also has space to put the resected specimen(s) without undocking.
In this first 100-case-series,all surgeries were completed without any intraoperative complications.Operative time was comparable to that of multi-port and SP extraperitoneal RARP approaches.Median estimated blood loss with SP TV was lower(100.0 mL with SP TV versus 200.0 mL with multi-port and 190.0 mL with SP extraperitoneal)compared to these techniques [12].The learning curve of an experienced robotic surgeon enriched plateau in the first 20 cases for console, dissection, and anastomosis times.
One of the main arguments against Retzius-sparing RARP is the index of positive margins.However, in our series,15.0% of patients had positive surgical margins, which is comparable to the 13.0% in standard multi-port transperitoneal RARP reported by a systematic review [13].Furthermore, none of the patients with positive margins have developed BCR thus far.The only patient with BCR inour series did not have positive margins; this patient had intermediate-risk disease preoperatively and extraprostatic extension on final pathology.

Table 1 Demographic and baseline characteristics(n=100).
One limitation of this surgical approach is the lymph node dissection.This is why patient selection is a crucial factor for the low rate of BCR seen in these patients.Furthermore, the nerve dissection and postoperative erectile recovery associated with this approach is comparable to that of traditional transperitoneal RARP.The three-day Foley catheter duration is an established goal and depends on tension of suture line, previous scar tissue, and the color of urine.If necessary, the catheter is maintained longer.The range of catheter duration in this series were from 2 days (1.0%) to 10 days (2.0%).For the initial cases in this series, the catheter was maintained around 10 days.After 15 cases and removal optimization,3 days became the standard duration.
An advantage of SP TV RARP is the time to urinary continence, obtained within 3 days after Foley removal in50.0% of the patients.These improved continence outcomes may be due to the avoidance of retropubic and perivesical structures during surgery; however, further analysis is required to determine the patient-related contributing factors.Sexual performance was also assessed, and it is evident that most patients need medication (PDE5 inhibitors) or intracorporeal injections to achieve mild to moderate ED(SHIM scores 12-16).Even so,it is noteworthy that 33.0%of the patients had moderate to severe ED prior to the surgery.

Table 2 Perioperative and pathology outcomes (n=100).
We acknowledge that the single surgeon and single-center status of this study is an important consideration.Consequently, additional comparative studies are necessary to clarify and confirm the promising early results at our institution.

Figure 6 Sexual function after transvesical single-port robot-assisted radical prostatectomy.ED,erectile dysfunction;PDE5, phosphodiesterase-5; SHIM, Sexual Health Inventory for Men.
5.Conclusion
SP TV RARP is a feasible approach for patients with clinically localized prostate cancer.In the first consecutive 100 cases, we reported favorable outcomes related to a short length of hospital stay, opioid-free recovery, and improved time to urinary continence.
Author contributions
Study concept and design: Jihad Kaouk.
Data acquisition: Roxana Ramos-Carpinteyro, Ethan L.Ferguson, Jaya S.Chavali, Albert Geskin.Data analysis: Roxana Ramos-Carpinteyro.
Drafting of manuscript: Roxana Ramos-Carpinteyro, Ethan L.Ferguson.
Critical revision of the manuscript: Jihad Kaouk.
Conflicts of interest
Dr.Jihad Kaouk is a consultant for Vascular Technology,Inc.(Nashua, NH,USA)and a speaker for Intuitive Surgical,Inc.(Sunnyvale,CA,USA).The other authors declare no conflict of interest.
 Asian Journal of Urology2023年4期
Asian Journal of Urology2023年4期
- Asian Journal of Urology的其它文章
- Robot-assisted adrenalectomy: Step-by-step technique and surgical outcomes at a high-volume robotic center
- The application of internal suspension technique in retroperitoneal robot-assisted laparoscopic partial nephrectomy with a new robotic system KangDuo Surgical Robot-01: Initial experience
- A systematic review of robot-assisted partial nephrectomy outcomes for advanced indications: Large tumors (cT2-T3), solitary kidney, completely endophytic, hilar,recurrent, and multiple renal tumors
- Three-dimensional automatic artificial intelligence driven augmented-reality selective biopsy during nerve-sparing robot-assisted radical prostatectomy:A feasibility and accuracy study
- Robot-assisted oncologic pelvic surgery with Hugo?robot-assisted surgery system: A single-center experience
- Prospective observational study on the prognosis of ureteral lesions caused by impacted stones via dual-energy spectral computed tomography
