Intermediate-term oncological and functional outcomes in prostate cancer patients treated with perineal robot-assisted radical prostatectomy: A single center analysis
Umberto Carbonara*, Giuseppe Lippolis, Luciano Rella,Paolo Minafra, Giuseppe Guglielmi, Antonio Vitarelli,Giuseppe Lucarelli, Pasquale Ditonno
Department of Emergency and Organ Transplantation, Urology Unit, Aldo Moro University, Bari, Italy
KEYWORDS Prostate cancer;Robotic;Perineal;Radical prostatectomy;Continence;Robot-assisted radical prostatectomy;Nerve-sparing
Abstract Objective: In the last 10 years,robotic platforms allowed to resume of some alternative surgical approaches, including perineal robot-assisted radical prostatectomy (p-RARP).Herein, we present in detail the oncological and functional outcomes of patients who underwent p-RARP with a median follow-up of 30 months.Methods: Patients presenting low- or intermediate-risk prostate cancer and prostate volume up to 60 mL who underwent p-RARP between November 2018 and November 2022 were selected.Baseline, intraoperative, pathological, and postoperative data were collected and then analyzed.Results: Thirty-seven p-RARP cases were included.Such patients presented mean age of 62 years and a mean Charlson comorbidity index of 4.Body mass index of ≥25 kg/m2 was reported by 24(64.9%)patients,as well as 7(18.9%)patients reported a past surgical history.Mean prostate volume and median prostate-specific antigen were 41 mL and 6.2 ng/mL, respectively.The median operative time was 242 min.The positive surgical margin rate was 45.9%.In terms of postoperative complications,10 patients reported complications with any grade;however,a single case (2.7%) of major (Clavien-Dindo grade ≥3) complication was observed.No patient with biochemical recurrence or distant metastasis was reported at 2 years of follow-up.Recovery of continence rates were 67.6%,75.7%,and 92.9%,at 6 months,12 months,and 24 months after surgery, respectively.Conclusion: p-RARP is a challenging but safe minimally invasive approach for selected patients with prostate cancer suitable for radical prostatectomy,showing outstanding functional recovery.Despite positive surgical margin rates being relatively high,no cases of biochemical recurrence or distant metastasis were reported after a median follow-up of 30 months.
1.Introduction
Radical prostatectomy(RP)is one of the primary options for the management of patients with localized prostate cancer(PCa) [1].RP performed with a perineal approach historically had been the standard technique for the removal of the entire prostatic gland.However,retropubic RP by Walsh[2] has progressively replaced perineal one as the widespread surgical treatment for patients with PCa given that retropubic RP overcomes the technical limits of perineal RP and offers more familiar landmarks [3,4].
Nowadays, the development of da Vinci robotic platforms significantly contributed to the rapid spread of robot-assisted RP (RARP) which is become “de-facto” the new standard in PCa treatment [5,6].The robotic system provides some technical benefits such as seven freedom degrees, filtration of the tremor, a magnified view, and improved ergonomics that enable urologists to resume and improve old-fashioned approaches [2,7,8], such as the perineal RP by Young [4].
To date, a number of early experiences with perineal RARP (p-RARP) were reported in the literature but only a few middle-term series have been published [9-11].Herein, we display in detail our series of p-RARP with median two-year follow-ups which were performed at an Italian tertiary center.
2.Patients and methods
2.1.Study design and population
The data are retrieved from a prospectively maintained database(IRB number:071337-30/09/2020-AOUCPG23/COMET/P;number of the study:6523).Patients with low-or intermediateriskPCaandprostate volumeupto60mLwhounderwentp-RARP between November 2018 and November 2022 at the Bari University Hospital (Bari, Italy) were identified.Patients who presented prostate volume greater than 60 mL, high-risk PCa,metastasis, risk of nodal metastasis, or locally advanced PCa were not included in the present analysis.Since p-RARP has limited surgical field,we excluded patients with an indication to locoregional lymph node dissection(LND),according to the current nomograms and guidelines[1,12](Table 1).Also,patients who underwent surgery for benign prostate hyperplasia were excluded[13].Preoperative multiparametric prostate magnetic resonance imaging was performed on the whole cohort.
A single expert surgeon (Ditonno P) completed more than 500 robotic cases (excluding robotic perineal prostatectomy) along with consolidated open expertise in the prostate, kidney, bladder, and transplant surgery [14].During all the procedures, there was the assistance of a perineal expert surgeon (Vitarelli A) with more than 200 perineal procedures(transperineal RP,genitourinary fistula repair, and transperineal approach to recalcitrant bladder neck contracture).
Da Vinci Xi?surgical system(Sunnyvale,California,USA)was used in all the cases [15].Patients who had preoperative erectile potency underwent bilateral or unilateral nerve-sparing p-RARP, except when there were contraindications according to current guidelines.European Association of Urology guidelines were also followed for the risk stratification [1].
These variables were presented in our perspective-maintained database:
?Baseline characteristics such as age, race, body mass index(BMI),American Society of Anesthesiologists(ASA),comorbidities, symptoms, history of prior surgery,preoperative prostate-specific antigen(PSA),ultrasound prostate volume, prostatic biopsy, clinical tumor, node,and metastasis (TNM) staging, preoperative International Prostate Symptom Score, International Index ofErectile Function-5 (IIEF-5), and history of urinary incontinence.
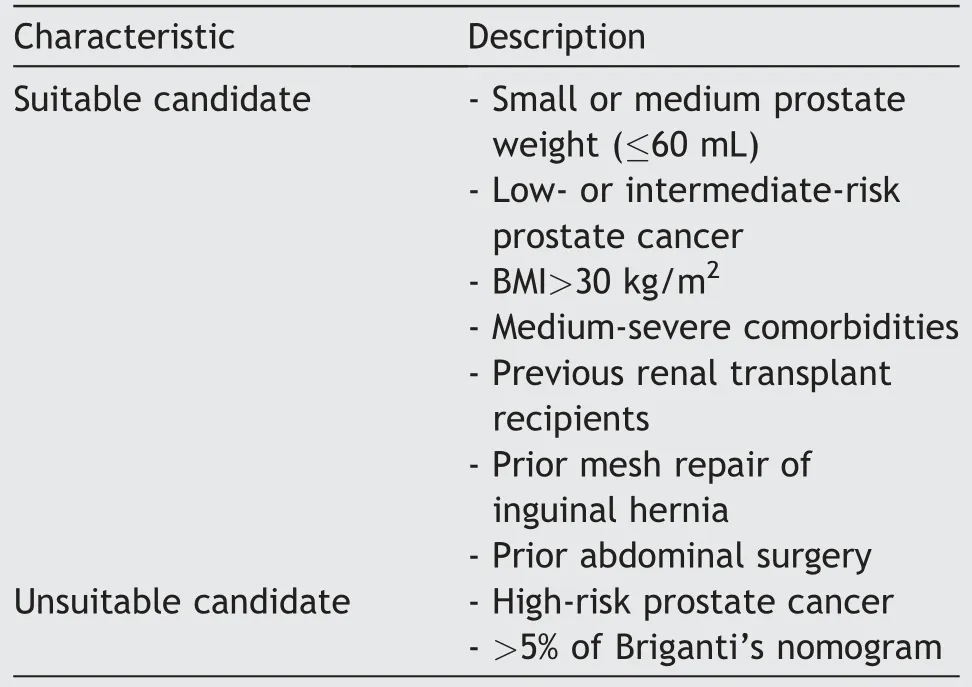
Table 1 Suitable candidates for perineal robot-assisted radical prostatectomy at Bari University Hospital (Bari,Italy) between November 2018 and November 2022.
?Treatment and perioperative outcomes such as operative time (OT), estimated blood loss (EBL), length of stay, discharge hemoglobin complications (intra- and post-operative, graded according to Clavien-Dindo classification and European Association of Urology classification [16,17]), and 30-day readmission.
?Pathological outcomes such as histology, pathological TNM [18], grading, margins status (which was defined as tumor cells touching the inked edge of the specimen),regardless of localization and International Society of Urological Pathology grade group.The cut-off considered for the definition of focal positive surgical margin(PSM) was a linear extension of ≤3 mm.
?Oncological and functional outcomes such as biochemical recurrence(BCR)are defined as a PSA level of>0.2 ng/mL at two consecutive measurements[1,19].Continence was defined as the use of one pad or saver-pad [20].Postoperative erectile function assessment was performed using the IIEF-5 questionnaire[21].Potency was defined as an IIEF-5 score of 17 or more with or without the use of phosphodiesterase type 5 inhibitors [21].Questionnaires were provided to the patients at each visit.
2.2.Surgical technique and anatomical landmarks
The surgical technique was already described in detail[22].Herein,we report the key points of p-RARP and anatomical landmarks (Figs.1 and 2).The perineal region presents a diamond shape delimited by the inferior margin of the pubic symphysis anteriorly, the tip of the coccyx posteriorly, the inferior margin of ischiopubic rami and ischial tuberosities anterolaterally, and the sacrotuberous ligaments posterolaterally.The perineal body occupies the middle point of the perineum.It is a fundamental landmark during the perineal prostatectomy since giving attachment to the superficial and deep portions of the external anal sphincter posteriorly, as well as bulbospongiosus, and superficial transverse perineal muscles anteriorly.Concerning the surgical technique, the patient was placed in a dorsal lithotomy position or with a 10-15-degree Trendelenburg with a cushion under the sacrum which facilitated perineum exposition.After performing a semicircular perineal incision between the two ischial tuberosities,just 2 cm over the anus on the midline line, the dissection was performed on a plane anterior to the external anal sphincter which allowed to smoothly open the ischio-rectal fossae on both sides.A GelPOINT? (Applied Medical, Rancho Santa Margarita,CA,USA)was allocated in a subcutaneous pouch.GelPOINT?enabled the placement of the robotic arms through just one perineal incision.The prostate dissection was performed mediolaterally and from the apex to the base, reducing the risk of neurovascular bundles damage.After opening the Denonvilliers’ fascia, vas deferens was recognized, clipped, and then removed as well as the seminal vesicle.At this point, the isolation of the dorsal aspect of the prostate was completed and the membranous urethra was dissected from the external urinary sphincter gently, isolating completely the prostate apex and maintaining the membranous urethra as long as possible.Notably, cold scissors only were used for incision of the urethra.The catheter was clipped and then cut, keeping the balloon inflated inside the bladder.The anterior aspect of the prostate was then isolated by lifting the endopelvic fascia and the dorsal venous complex, preserving the Retzius space and its ligamentous structures.The ventral circular fibers of the bladder neck were identified and incised.After catheter removal,the incision of the bladder neck was completed on the lateral and dorsal margins.The anastomosis was executed through a running suture with unidirectional barbed suture (V-Loc? 180, Covidien,Mansfield, MA, USA) according to the single-knot method described by Van Velthoven et al.[23].

Figure 1 Perineal region illustrations.(A) Perineal region-can be described as a diamond shape delimited,anteriorly by the inferior margin of pubic symphysis (a), posteriorly by the tip of the coccyx (b), anterolaterally by the inferior margin of ischiopubic rami and ischial tuberosities (c),and posterolaterally by the sacrotuberous ligaments (d); (B)Skin incision.The black dished line is a semicircular landmark draw between the ischial tuberosities, 2 cm above the anus.A line of about 7 cm is measured as a chord of the previous line(black line).The red dashed line shows the skin incision.
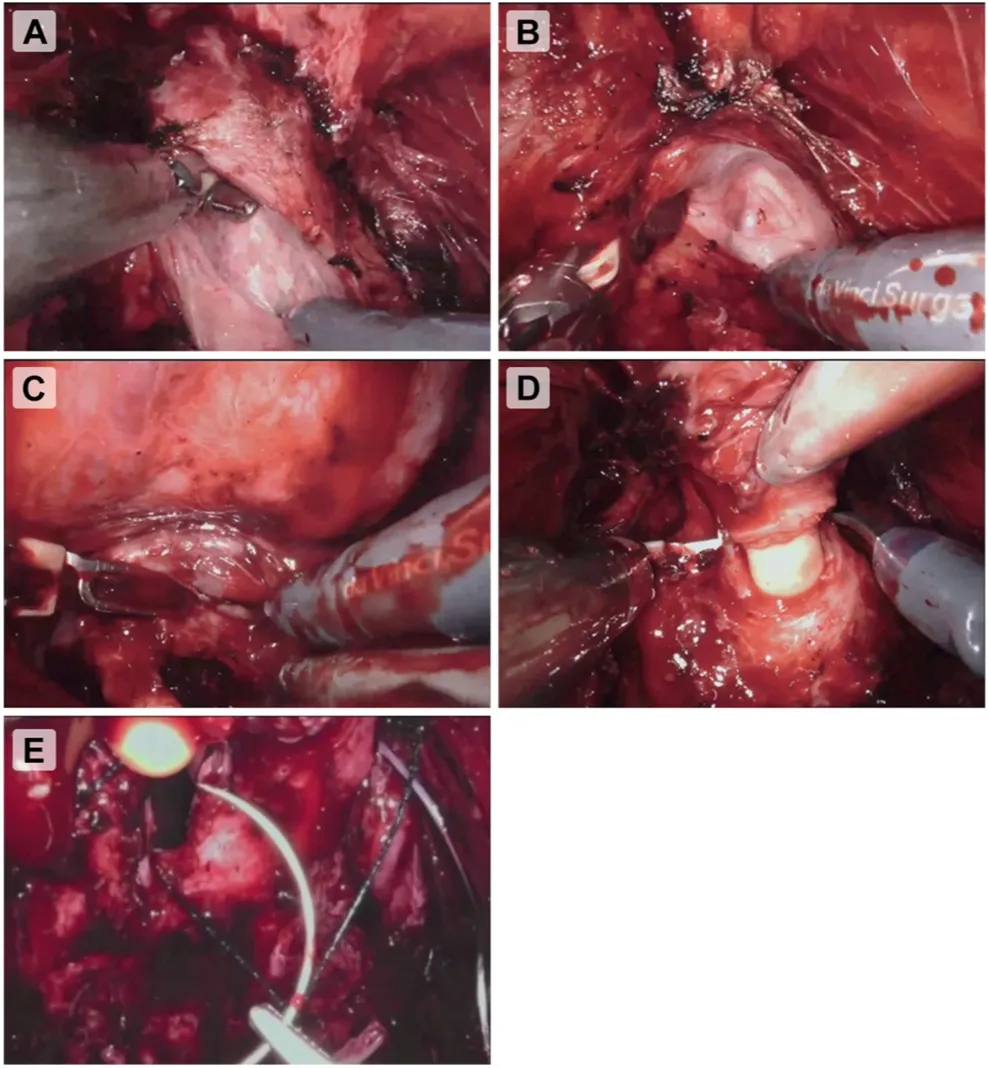
Figure 2 Intraoperative illustrations.(A) The retrograde dissection of the posterior surface of the prostate gland in the nerve-sparing approach; (B) Identification and dissection of lateral aspects of prostate gland; (C) Identification and dissection of seminal vesicles; (D) Incision of the membranous urethra; (E) Vesicourethral anastomosis.
2.3.Statistical analysis
Statistical analysis was conducted following guidelines[24].Patients’ characteristics and surgical outcomes were described using descriptive statistics.Medians with interquartile ranges (IQRs) and frequencies were adopted to report continuous and categorical variables,respectively.It was impossible to perform Kaplan-Meier analysis of recurrence-free survival, as well as overall and cancer survival, given that only a single case of death was observed.Moreover, no cancer-specific death or recurrences were reported among our cohort.All statistical tests were performed with SPSS?(Version 26.0, IBM Corp.,Armonk, NY, USA) and statistical significance was set at p<0.05.
3.Results
3.1.Baseline and staging characteristics
Overall, the outcomes of thirty-seven patients who underwent p-RARP were analyzed.Table 2 summarizes the baseline characteristics of the study population that reported mean age of 62(standard deviation[SD]5)years.Moreover,24(64.9%)patients showed BMI of 25 kg/m2or more,and 31(83.8%) patients reported ASA score of ≥2.History of pastabdominal surgical procedures was present in 4 (10.8%) patients with a single case of kidney transplantation.Mean prostate volume was 41 (SD 6) mL and median PSA was 6.2(IQR 4.8-7.6)ng/mL.Thirty-two(86.5%)of p-RARP patients had clinical T1c stage.Finally, 56.8% presented an International Society of Urological Pathology grade group of 1.
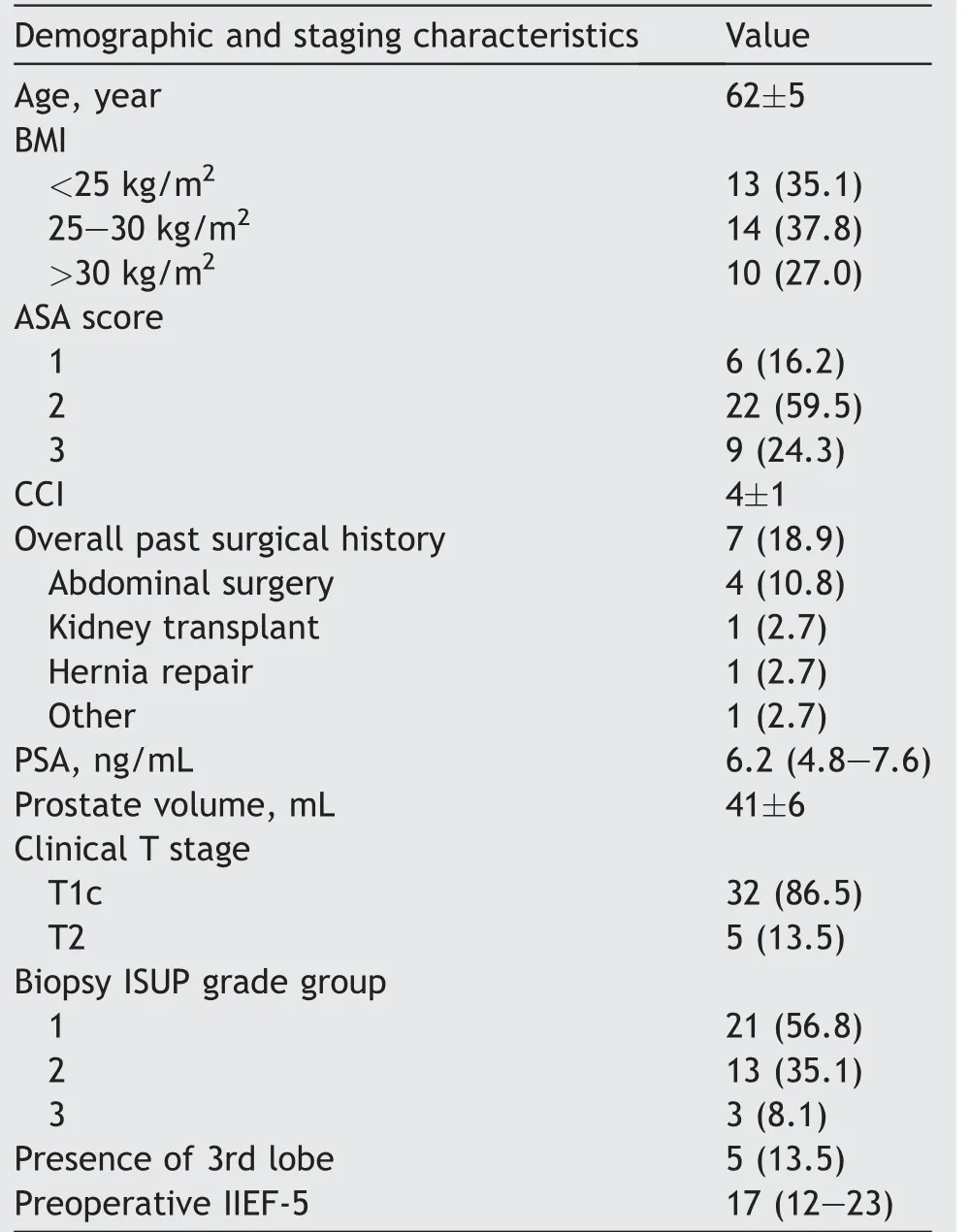
Table 2 Demographic and staging characteristics of patients undergoing p-RARP (n=37).
3.2.Surgical and pathology outcomes
Table 3 summarizes the intraoperative, postoperative, and anatomopathological characteristics.Median OT and EBL were 242 (IQR 202-282) min and 250 (IQR 150-350) mL,respectively.In terms of complications, 5 (13.5%) and 10 (27.0%) patients had intraoperative and overall postoperative complications, with a single case (2.7%) having a major complication (bleeding which required surgical management).Further details on surgical complications are provided in Supplementary Tables 1 and 2.Mean drain time,length of stay,and catheterization time were 1 day,3 days,and 7 days,respectively.PSMs were presented in 17(45.9%)patients.
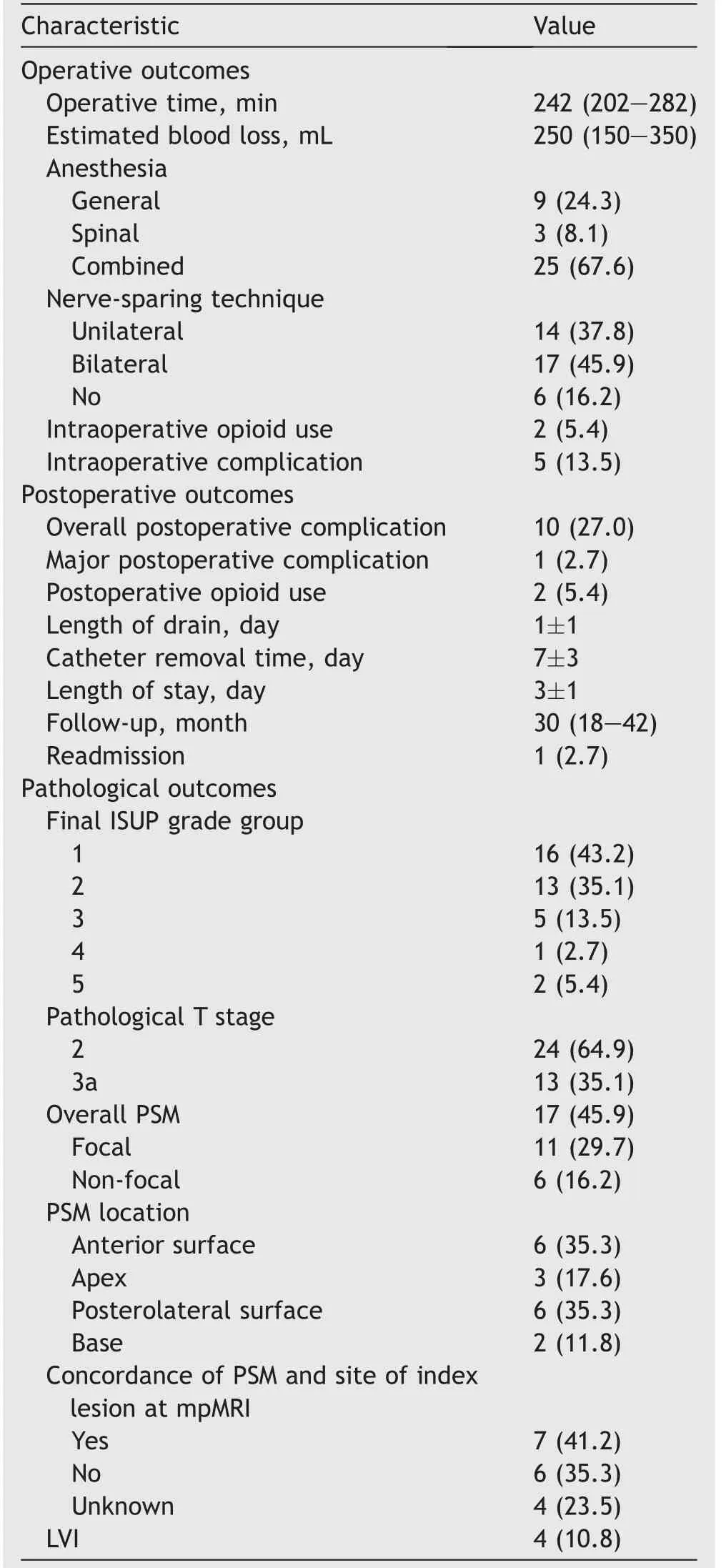
Table 3 Operative, postoperative, and histopathological outcomes of patients undergoing perineal robot-assisted radical prostatectomy (n=37).
3.3.Oncology and functional outcomes
Oncological and functional results are displayed in Table 4.Overall, no patients with BCR and distant metastasis werereported within 2 years of follow-up.Erectile function recovery rate increased from 64.9%at 6 months to 82.1%at 2 years after p-RARP.Similarly, an improvement in continence rate was observed over time from 67.6%to 92.9%at 6 months and 2 years of follow-up, respectively.
4.Discussion
Herein, we reported 2-year functional and oncological outcomes of patients who underwent p-RARP.To the best of our knowledge, it is the longest follow-up for this specific robotic procedure (Table 5) [11,25].More and more efforts are being made to develop and improve Retzius-sparing RARP approaches with the main aim of reaching an improvement in patients’ functional outcomes [26].As a matter of fact,p-RARP can be considered a Retzius-sparing robotic prostatectomy since it ensures that the anterior support structures of the bladder remain intact.Therefore,we believe that this work can make a crucial contribution to this topic [2].
In terms of patient selection, it is interesting to note that 64.9% of patients presented BMI of ≥25 kg/m2and 24.3% of patients presented ASA of >2.While 34.5% of patients had a history of surgery in our previous series [22],this percentage decreased to 18.9% in the update.This finding can be explained by the fact that the indications ofp-RARP are progressively expanded to include other types of patients, even without a past history of surgical procedures[2].Another advantage is that neuraxial or general anesthesia can be used according to patients’ medical and surgical history [27].
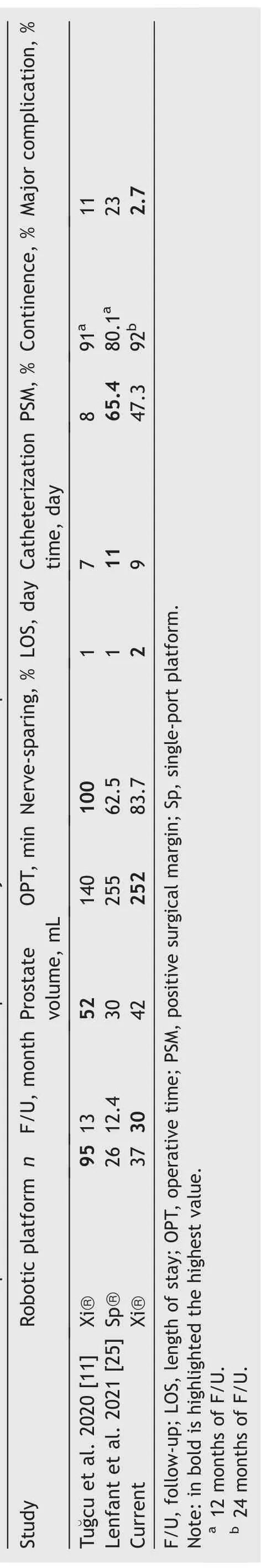
Table 5 Previous studies of perineal robot-assisted radical prostatectomy with more than 20 patients.
From a technical point of view, the nerve-sparing approach represents one of the challenging steps in p-RARP.One of the advantages of robotic platform consists of facilitating bundle dissection without losing adherence to key oncological principles [11,28].Moreover, p-RARP displays safe and effective outcomes in terms of median OT(242 min), EBL (250 mL), and low rates of overall complications(27.0%).It can be speculated that OT can be longer than those reported in the literature for standard RARP[6].However, it is mainly due to the open approach which considerably extends the OT and requires also perineal expertise [2].
Regarding perineal LND, we consciously selected patients who were not suitable for LND according to Briganti’s nomogram and staging at our institution.Concerns are still made about the safety and technical feasibility of this specific step [2].However, it can be reasonably assumed that the single-port da Vinci platform could facilitate LND with perineal approaches as reported by the Cleveland Clinic group and other groups worldwide [25,29].
In terms of oncological outcomes, there is no denying that our cohort showed a high rate(45.9%) of patients with PSM, 29.7% and 16.2% were focal and non-focal, respectively.In the largest series available to date about p-RARP,Tu?gcu et al.[11]presented the outcomes of 95 p-RARP cases from 2016 to 2018, showing that only 8 (8.4%) patients presented PSM after the surgical procedure.This difference can be explained by different phases of learning curves, as well as patients’ selection [2,11,30].Perhaps it was shown that a low prostate weight is considerably associated with high PSM rates[31-33].Moreover, patients who underwent full or partial nerve-sparing procedure and who received full bladder neck preservation had an almost two-fold higher probabilities of harboring PSMs at final pathology[31,34].Nevertheless,it is surprising to observe that despite the fact that there is a high rate of PSM among the cohort,there were no cases of BCR (defined as a PSA level of>0.2 ng/mL at two consecutive measurements) or distant metastasis at 24 months of follow-up.PSMs are considered one of the powerful predictors of BCR after RALP, even though apical PSMs have a relatively less predictive power of BCR [35].However, worse clinical stage and biopsy Gleason score are also associated with pathologic outcomes and BCR-free survival rates in patients with positive apical margins only [35].Such an aspect can be a plausible explanation to explain the lack of patients with BCR in our series since the inclusion criteria bring to the inclusion of patients with low- or intermediate-risk PCa and Gleason score at least of 7.Dell’Oglio et al.[26] recently published an interesting series of patients with high-risk PCa who underwent Retzius-sparing RARP.They found PSM rate of 28.8% and 4-year probability of freedom from BCR of 63.6%which is completely in line with previous studies on high-risk PCa patients who underwent an anterior RARP approach[36].Interestingly,they showed that high-grade disease and PSMs were independent predictors of inferior BCR and additional treatment after Retzius-sparing RARP [26].
Concerning functional outcomes, we demonstrate that recovery of continence (defined as the use of one pad or saver-pad)was relatively in line or even better compared to those reported in the literature in medium follow-up [6].After p-RARP, we observed a recovery of continence of 75.7% and 92.9% at 1 year and 2 years of follow-up,respectively.However, one of the largest series on anterior RARP showed a recovery of 85.2%at 1 year and 89.1%at 2 years of follow-up [37].Egan et al.[38] compared the outcomes of 70 patients who underwent Retzius-sparing RARP to those of 70 undergoing standard RARP.In their cohort, the authors showed that the Retzius-sparing approach, when compared to the standard approach, had a significant improvement in continence at 12 months(97.6% vs.81.4%, p=0.002), together with a faster return to continence(zero to one safety pad,44 days vs.131 days,p<0.001).The anatomical preservation of anterior ligaments and the attempt to maintain as much normal pelvic anatomy as possible allow reaching these functional results with our technique,similar to those of Retzius-sparing RARP[39,40].
Our study must be interpreted in light of its limitations.Firstly, our findings were derived from a retrospective review of prospectively collected observational data.A selection bias can be related to the patients’ selection criteria.Secondly, our findings were derived from a center with a relative reduction of surgical activity during COVID-19 pandemic [41].
5.Conclusion
p-RARP is still a challenging but safe minimally invasive approach for selected patients with outstanding functional recovery.Despite PSM rates being relatively high, no cases of BCR or distant metastasis were reported after 24 months of follow-up.p-RARP might be a valid alternative in patients with previous history of abdominal surgery, cardiac or pulmonary comorbidities,or in which the transperitoneal approach is not indicated.
Author contributions
Study concept and design: Umberto Carbonara.
Data acquisition: Umberto Carbonara, Giuseppe Lippolis,Luciano Rella, Paolo Minafra.
Data analysis: Umberto Carbonara.
Drafting of manuscript: Umberto Carbonara.
Critical revision of the manuscript: Umberto Carbonara,Giuseppe Lippolis, Luciano Rella, Paolo Minafra, Giuseppe Guglielmi, Antonio Vitarelli, Giuseppe Lucarelli, Pasquale Ditonno.
Conflicts of interest
The authors declare no conflict of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2023.05.005.
 Asian Journal of Urology2023年4期
Asian Journal of Urology2023年4期
- Asian Journal of Urology的其它文章
- Robot-assisted adrenalectomy: Step-by-step technique and surgical outcomes at a high-volume robotic center
- The application of internal suspension technique in retroperitoneal robot-assisted laparoscopic partial nephrectomy with a new robotic system KangDuo Surgical Robot-01: Initial experience
- A systematic review of robot-assisted partial nephrectomy outcomes for advanced indications: Large tumors (cT2-T3), solitary kidney, completely endophytic, hilar,recurrent, and multiple renal tumors
- Three-dimensional automatic artificial intelligence driven augmented-reality selective biopsy during nerve-sparing robot-assisted radical prostatectomy:A feasibility and accuracy study
- First 100 cases of transvesical single-port robotic radical prostatectomy
- Robot-assisted oncologic pelvic surgery with Hugo?robot-assisted surgery system: A single-center experience
