Double-face urethroplasty in patients with obliterative bulbar strictures post-transurethral resection of the prostate mid-term outcomes in high-volume referral center
Pnkj M.Joshi ,Mnuel Hevi *,Ytm Lkshmi Sreerng ,Mro Bndini , Amey Ptil , Shreys Bhdrnvr ,Vipin Shrm , Sndeep Bfn , Snjy B.Kulkrni
a Kulkarni Reconstructive Urology Center, 3, Rajpath Society, Paud Road, Pune 411038, India
b Urology Department, Ramo′n y Cajal University Hospital, IRYCIS, University of Alcala′, Madrid, Spain
c Urological Research Institute (URI), Unit of Urology, IRCCS Ospedale San Raffaele, Vita Salute, San Raffaele University, Milan, MI, Italy
KEYWORDS Double-face urethroplasty;Obliterative urethral stricture;Post-transurethral resection of prostate;Urethral stricture;Spongiofibrosis;Iatrogenic stricture
Abstract Objective: Incidences of post-transurethral resection of the prostate (post-TURP)strictures are between 2.2% and 9.8%.Stricture commonly occurs within the first 6 months.Our objective was to assess the outcomes of patients with obliterative strictures post-TURP that underwent a double-face urethroplasty.Methods: This is a single-center prospective study of 17 patients with obliterative proximal bulbar stricture post-TURP who underwent double-face graft urethroplasty by two surgeons between January 2014 and January 2020.We defined post-TURP obliterative strictures as those patients who presented with complete or almost complete obstruction of the urethral lumen and who have had a history of acute urine retention.We have excluded patients with bladder neck contracture.Primary outcome was treatment success,defined as the no need for further treatments.Secondary outcome was post-urethroplasty continent rate.Results: Seventeen patients were included in the study with median age of 66 (interquartile range 40-77)years;median time of follow-up was 24(interquartile range 12-84)months;median stricture length was 4 (interquartile range 2-6) cm.Of the 17 patients, 15 (88.2%) were successful.All patients were continent after urethroplasty.Conclusion: With mid-term follow-up, treatment of obliterative proximal bulbar strictures with double-face buccal mucosa graft is a safe and effective procedure.Obliterative proximal bulbar strictures merit double-face urethroplasty with high-rate success and functional outcomes.
1.Introduction
Urethral stricture is a well-known complication in patients undergoing transurethral resection of the prostate (TURP)with an incidence of around 4.1% [1].True incidences of post-TURP strictures are underreported.There are few series with extended follow-up reported incidences of urethral strictures between 2.2% and 9.8% [2].Most of the patients present within 6 months of TURP[3].Fenton et al.[4] in 2005 reported that of 194 patients with urethral stricture, 63 (32.5%) were classified as iatrogenic, with TURP being the most frequent cause(26/63,41.3%).In the clinical trial conducted by Komura et al.[5], it was found that the urethral stricture rate was notably higher in the bipolar TURP resection group compared to monopolar TURP for prostates larger than 70 mL (20% in bipolar TURP vs.2% in monopolar TURP).There were no differences for prostates smaller than or equal to 70 mL.Whatever may be the type of energy used or technique used for TURP,stricture still is a known occurrence.
Post-TURP stricture can occur at any site in the urethra,most commonly seen in the navicular fossa and bulbar urethra[6].The etiology of post-TURP stricture is probably due to multiple causes, including improper traumatic insertion of the resectoscope, prolonged resection time,ischemia, prolonged catheterization, and infection.However, the main cause of stricture post-TURP remains undetermined [7,8].True membranous urethral stricture does not occur after TURP.These are actually very proximal bulbar strictures.It was considered a reconstructive challenge in these patients as the internal sphincter mechanism (bladder neck) became non-functional and urinary continence relied on the rhabdosphincter or membranous urethra [6,9].
According to our experience,we consider that these are proximal bulbar strictures, not strictly sphincter stenoses,although different authors described them as bulbomembranous or sphincteric strictures [3,10,11].It was feared that urethroplasty in these patients could cause damage to the external urethral sphincter and a high rate of incontinence[10].Several techniques have been described for the treatment of stenosis in the proximal bulbar urethra,ranging from excision and anastomosis to graft urethroplasty [12].In these patients who do not have the internal sphincter mechanism,the excision anastomosis is not a valid option due to the possibility of damaging the sphincter in addition to affecting sexual function due to vascular damage when transecting the urethra [13].In patients with obliterative strictures at the level of the proximal bulbar urethra, which are too severe for a simple one-side grafting, urethroplasty with a double-face graft without transecting is an adequate option because it provides us with a good urethral caliber in addition to avoiding compromise of sexual function [13-15].
Recently Go′mez et al.[6] have described an intrasphincteric anastomotic urethroplasty technique especially useful for patients who have undergone TURP, achieving a continence rate of 85%.They performed a careful dissection between the rhabdosphincter muscle fibers and the urethra which allowed them to perform an excision and anastomosis while preserving the sphincter.This technique was developed based on the anatomical discovery made by Dalpiaz et al.[16].In the anatomical and histological study carried out, the existence of a thin layer of connective tissue that separates the membranous urethra from the rhabdosphincter was demonstrated.Ventral onlay is a established technique now for such proximal post-TURP strictures.However, it works better in non-obliterative strictures.We suggest that obliterative strictures need a double-face urethroplasty.
The aim of this study was to assess long-term outcomes in patients with obliterative strictures post-TURP that underwent double-face graft urethroplasty.Furthermore, we aimed to evaluate independent risk factors that influence on urethroplasty failure.
2.Patients and methods
2.1.Patient population and study design
After institutional review board approval (07/21), we performed an observational, descriptive, and prospective study on a cohort of patients with obliterative proximal bulbar strictures post-TURP that underwent a double-face urethroplasty between January 2014 and January 2020 in a tertiary referral center of reconstructive urethral surgery(Kulkarni Reconstructive Urology Center,Pune,India).Tight stricture was defined by Palminteri et al.[13] as a very narrow urethral plate with width less than 3 mm.We defined obliterated stenosis as those patients after undergoing TURP who presented a complete or almost complete obstruction of the urethral lumen and who have had a history of acute urine retention.
All surgical procedures were performed by two urologists (Joshi PM and Kulkarni SB).Inclusion criteria of study were obliterative proximal bulbar strictures post-TURP treated with double-face urethroplasty.Patients with bladder neck contracture, preoperative urinary incontinence,or follow-up less than 12 months were excluded.All patients signed a dedicated informed consent.Following variables were recorded: demographic data, details of TURP, urethral stricture length, bladder catheter time,and follow-up.No intervention was done before 3 months of previous TURP.
Stricture location was classified with endoscopy (Fig.1)and urethrography (Fig.2).All surgeries were performed under spinal plus general anesthesia.The primary outcome of study was treatment success,defined as the no need for further treatments.Secondary was evaluation of postoperative urinary incontinence, defined as the no need to wear pad, even security pad.
2.2.Preoperative investigation
The detailed clinical history and physical examination were performed on all patients.The type of previous prostatic surgery was collected (bipolar and holmium laser).Retrograde urethroscopy and fluoroscopic retrograde urethrogram were performed in all patients to demarcate the location and length of the stricture.Urine culture was routinely obtained.
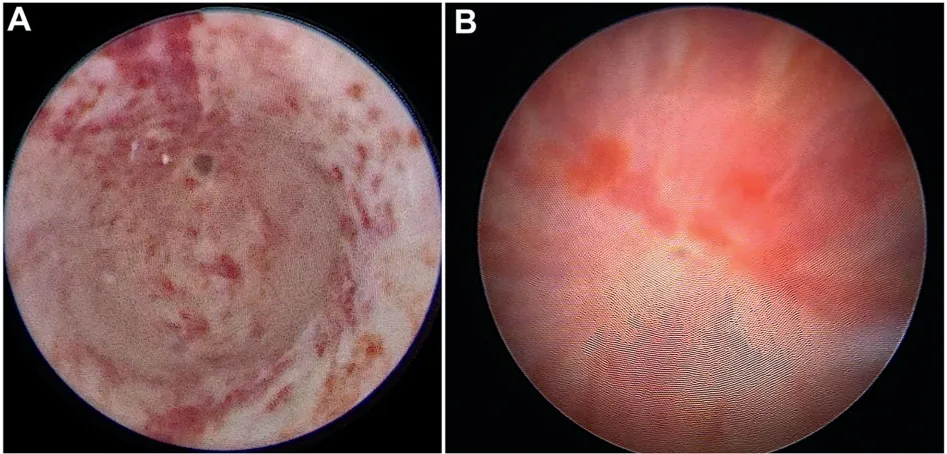
Figure 1 Endoscopic view of proximal bulbar obliterative stricture.(A)Retrograde endoscopy of bulbar urethral stricture with minimum passage (<3 mm); (B) Endoscopy of complete obliterative bulbar urethral stricture.

Figure 2 Urethrogram of obliterative stricture at bulbar urethra post-transurethral resection of the prostate.
2.3.Surgical technique
Intraoperative endoscopy was performed with a 4.5 Fr ureteroscope.The urethral stricture was identified.Occasionally there was a very small passage and a guidewire was passed across the stricture into the bladder (Fig.3A).These strictures are usually very proximal and close to membranous urethra and the sphincter[3].Methylene blue was injected into the urethra (Fig.3A).Midline perineal incision was made.Bulbospongiosus muscle was incised in midline and bulbar urethra was identified (Fig.3B).The urethra was incised ventrally at 6 o’clock position over a dilator and the urethrotomy was continued proximally and distally (Fig.3C and D).
We used an ophthalmic scalpel to incise the urethra ventrally.We took stay suture to retract the urethra(Fig.3E and F).The urethrotomy was extended till good pink urethral mucosa was seen.DeBakey forceps inside the urethra was useful(Fig.3G).Once the urethral lumen was adequate,the proximal part of the graft was sutured on its ventral face(Fig.3H).A nasal speculum was passed through the urethra and a dorsal inlay incision made across the obliterated urethral plate(Fig.4A and B).Then,we inserted a small buccal mucosa graft as a dorsal inlay[17](Fig.4C).The dorsal inlay graft was quilted with a Vicryl?tacker (Absorbatack 710,Medtronic Parkway, Minneapolis, MN, USA) [18] (Fig.4D).Suturing of the graft in the ventral position was completed with two running sutures (Fig.5A).The spongy tissue was sutured to cover the ventral urethral part(Fig.5B).
For patients who still preserved urethral lumen, a ventral onlay urethroplasty was enough to provide width caliber to the urethra, but in patients with obliterative strictures, Joshi PM proposed a double-face urethroplasty.It took about 10 min operative time to insert a dorsal inlay graft.
2.4.Postoperative course and follow-up criteria
The bladder catheter was removed 4 weeks after surgery.Subsequently, a uroflow was performed; and if there were no voiding problems,the suprapubic catheter was removed 1 week later.All patients received low dose antibiotics until catheter was removed.Urethroplasty failure was considered in patients that required postoperative procedures,including dilations.
Follow-up visits were scheduled every 3 months during the first year and annually later.Medical visit included clinical history, assessment of lower urinary tract symptoms, physical examination, and uroflow.Any decrease in urinary flow was evaluated with retrograde urethrography,and an endoscopy or urodynamic study would be done if necessary.Follow-up period was defined as the time from surgery to the last clinical control or failure event.
3.Results

Figure 3 Urethral dissection and ventral approach.(A) The 3 Fr guide-wire and methylene blue were inserted through the urethra; (B) Bulbospongiosus muscle was incised in midline; (C and D) The urethra was incised ventrally over a dilator and the urethrotomy was continued proximally and distally;(E and F)The urethra was incised and a stay suture was taken from the urethra,through the spongy tissue, very close to the mucosa and held apart; (G) The urethrotomy was extended till good pink urethral mucosa was seen; (H) Proximal part of the graft was sutured on its ventral face.
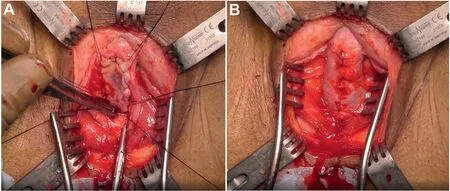
Figure 5 Ventral graft and urethral closure.(A) The ventral graft sutured with two running sutures; (B) Spongy tissue sutured to cover the graft.
Descriptive data of patients are described in Table 1.Seventeen patients with obliterative proximal bulbar stricture post-TURP were treated with double-face buccal mucosa graft from January 2014 to January 2020.Sixteen(94.1%) patients underwent TURP (bipolar) and one (5.9%) patient underwent HOLEP.Six (35.3%) patients underwent suprapubic catheter placement before surgery.Median patient age was 66 (interquartile range [IRQ]40-77) years, and median stricture length was 4(IQR 2-6) cm.Twelve (70.6%) patients have undergone previous treatments; 10 (58.9%) patients have undergone direct vision internal urethrotomy, and dilatation occurred in 2 (11.8%) patients.Median preoperative maximum flow rate(Qmax)was 7(IQR 3-8)mL/s.Median hospital stay was 2 (IQR 2-4) days.There were no early (<30 days) postoperative complications.Median bladder catheter time was 30 (IQR 28-35) days.Median follow-up was 24 (IQR 12-84)months.No patient was lost to follow-up.Fifteen (88.2%)patients were classified as a success and 2 (11.8%) as a failure.Median postoperative Qmaxwas 24(IQR 8-32)mL/s;median graft length was 7 (IQR: 7-9) cm and median graft width was 2.0 (IQR 1.5-2.0) cm.
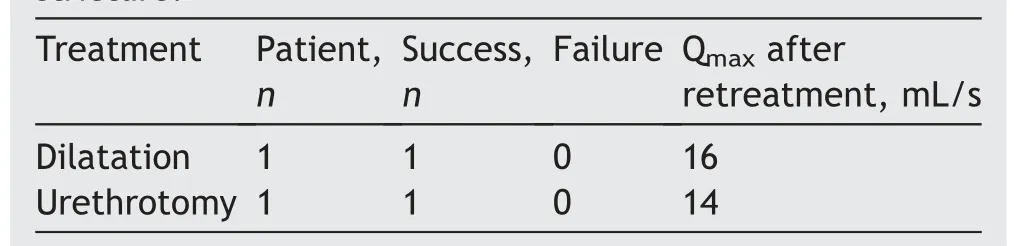
In patients in whom surgery failed, recurrence occurred during the first year.All patients were continent after surgery and until the last medical visit.The treatment of patients with recurrent urethral stricture is summarized in Table 2.We did not observe any complications in relation with oral harvesting.
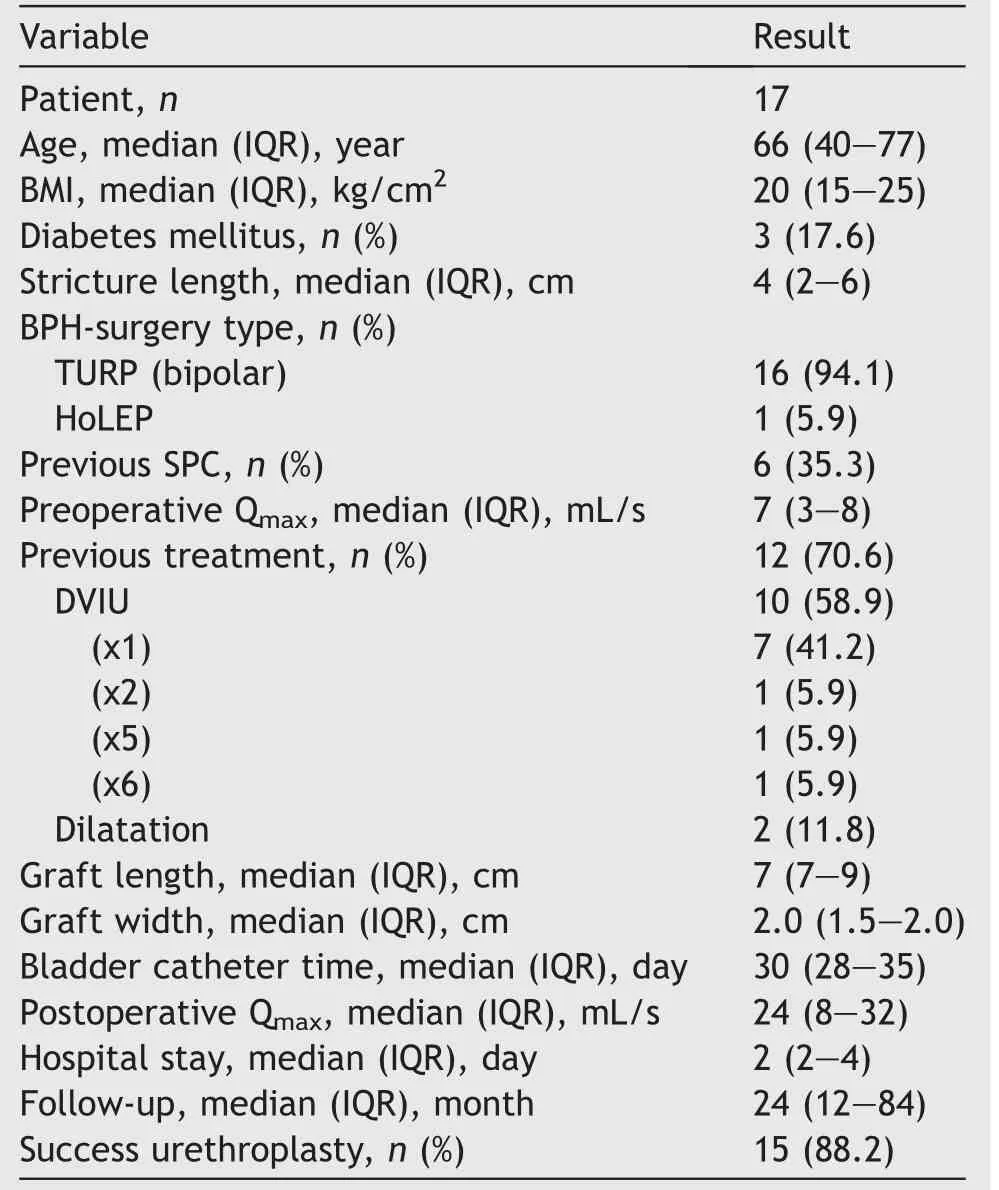
Table 1 Patient characteristics.
Qmax, maximum flow rate.
4.Discussion
Urethral stricture in patients undergoing TURP is a well-known complication with incidences between 2.2%and 9.8% of these patients [2].The most frequent site of appearance of the stricture is the meatus followed by the bulbar urethra.Although most studies have called these strictures as sphincter strictures,in our experience they are proximal bulbar urethral strictures [3].The repair of strictures in the proximal bulbar urethra in patients undergoing TURP continues to be a great reconstructive challenge due to the risk of sphincter damage after repair.In these patients, the internal sphincter mechanism was lost; therefore, continence depends on the external sphincter [8].Despite numerous anatomical studies on the male external urethral sphincter, it still remains a controversial subject[9,19,20].
There are two mechanisms that ensure continence in men.The first of them corresponds to the smooth muscle fibers of the detrusor muscle at the level of the bladder neck.The rhabdosphincter,on the other hand,is composed of striated muscle fibers that extend from the base of the bladder to the urogenital diaphragm [8,10,19,21].
The rhabdosphincter is about 2 cm long and is found surrounding the membranous urethra with an omega-shaped inserting dorsally at the perineal body via a tendinous raphe, with shortage of fibers in the ventral part [8,21].
Innervation of the rhabdosphincter comes from the pelvic (autonomic) and pudendal (somatic) branches which enter into the sphincter in posterolateral area [20].According to the anatomical descriptions of Strasser et al.[21]and the pattern of the rhabdosphincter forming an omega-shaped, ventral and ventrolateral dissection is relatively safe as there is a shortage of muscle fibers in this area [8].Excessive dissection at the dorsal level or transecting urethroplasty techniques in patients undergoing TURP can damage the sphincter striated fibers and consequently leave these patients incontinent [5,10,22].
Traditionally, short and obliterative urethral strictures have been treated by excision and anastomosis, although the consequences of vascular damage and urethral shortening with this technique have promoted the trend to treat these patients with augmented urethroplasty, even in the shortest strictures [12,13].Recently, Favre et al.[23] have published a series of 77 patients with bulbomembranous urethral stricture after TURP treated with anastomotic urethroplasty with a postoperative continence rate of 92%.In this sense, the publication by Go′mez et al.[6] in 2020 proposed to perform a careful dissection of the membranous urethra with preservation of the striated sphincter,which allowed an excision and anastomosis to be performed with continence rates around 85%.
Classically, in patients with proximal bulbar urethral strictures, close to the sphincter, the preferred treatment is the ventral onlay buccal mucosa graft technique [3,24].However, for patients with obliterative strictures with complete obstruction of the urethral lumen, one-side graft urethroplasty may be insufficient to provide an adequate caliber to the urethral lumen [13].According to Kulkarni et al.[3], once the urethral ventral face was open, an incision was made on the ventral face at 6 o’clock until the underlying spongy tissue was visualized.With this approach,damage to the sphincter fibers is avoided since it is absent on its ventral side; therefore, there is no risk of postoperative incontinence with the ventral onlay urethroplasty technique.
Dorsal approach would involve a full thickness urethrotomy and this would possibly cause incontinence as the stricture is close to membranous urethra.Gimbernat et al.[25]reported a continence rate of around 93%in a study of 14 patients.
The novelty introduced by us is the fixation of the dorsal inlay graft with Vicryl?tacker first described by Joshi et al.[18], since in very proximal strictures the quilting of the graft becomes challenging.According to our experience and what has been previously reported in the literature,double-face urethroplasty has allowed us to achieve a success rate of 88%, so we propose that it be the chosen technique for these patients that undergoing TURP with obliterative strictures.Our study is limited by the results of a single institution and with a small sample of patients.However, we cannot perform a comparative statistical analysis with other techniques as it is not prudent to perform dorsal approach.
5.Conclusion
Proximal bulbar strictures are treated with ventral approach.Obliterative strictures should be treated with double-face (ventral onlay with dorsal inlay buccal graft)urethroplasty technique.This technique has a high success rate and maintains continence.
Author contributions
Study design: Pankaj M.Joshi.
Data acquisition: Pankaj M.Joshi, Manuel Hevia, Yatam Lakshmi Sreeranga, Marco Bandini, Amey Patil, Sandeep Bafna, Vipin Sharma, Sanjay B.Kulkarni.
Data analysis: Pankaj M.Joshi, Manuel Hevia, Marco Bandini, Shreyas Bhadranavar.
Drafting of manuscript: Pankaj M.Joshi, Manuel Hevia.
Critical revision of the manuscript:Pankaj M.Joshi,Manuel Hevia.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2023年4期
Asian Journal of Urology2023年4期
- Asian Journal of Urology的其它文章
- Robot-assisted adrenalectomy: Step-by-step technique and surgical outcomes at a high-volume robotic center
- The application of internal suspension technique in retroperitoneal robot-assisted laparoscopic partial nephrectomy with a new robotic system KangDuo Surgical Robot-01: Initial experience
- A systematic review of robot-assisted partial nephrectomy outcomes for advanced indications: Large tumors (cT2-T3), solitary kidney, completely endophytic, hilar,recurrent, and multiple renal tumors
- Three-dimensional automatic artificial intelligence driven augmented-reality selective biopsy during nerve-sparing robot-assisted radical prostatectomy:A feasibility and accuracy study
- First 100 cases of transvesical single-port robotic radical prostatectomy
- Robot-assisted oncologic pelvic surgery with Hugo?robot-assisted surgery system: A single-center experience
